Tick-borne diseases represent a significant public health concern. The links at the end of this Substack send you to my detailed entries on Lyme disease, babesiosis, and Bartonellosis--and now it’s time to talk about ticks and other species that pose a danger in the springtime.
These are the bacteria belonging to the genera Ehrlichia and Anaplasma. They transmit bacterial pathogens responsible for a spectrum of illnesses with overlapping symptoms, making accurate diagnosis and timely treatment crucial to prevent severe complications. As the weather warms, the risks become even greater.
As you will see, Ehrlichiosis and Anaplasmosis share overlapping symptoms and lab results, particularly in early stages. The same laboratory abnormalities can be seen in other early tick-borne infections including Borrelia miyamotoi (hard tick relapsing fever), rickettsial infections (Rickettsia rickettsii, Rocky Mountain Spotted fever; Rickettsia parkerii; Coxiella burnetti, Q-fever), as well as tick-borne viral infections including the Heartland and Bourbon viruses. Babesiosis may even occasionally cause the same blood abnormalities.
You Don’t Want to Get Ehrlichiosis
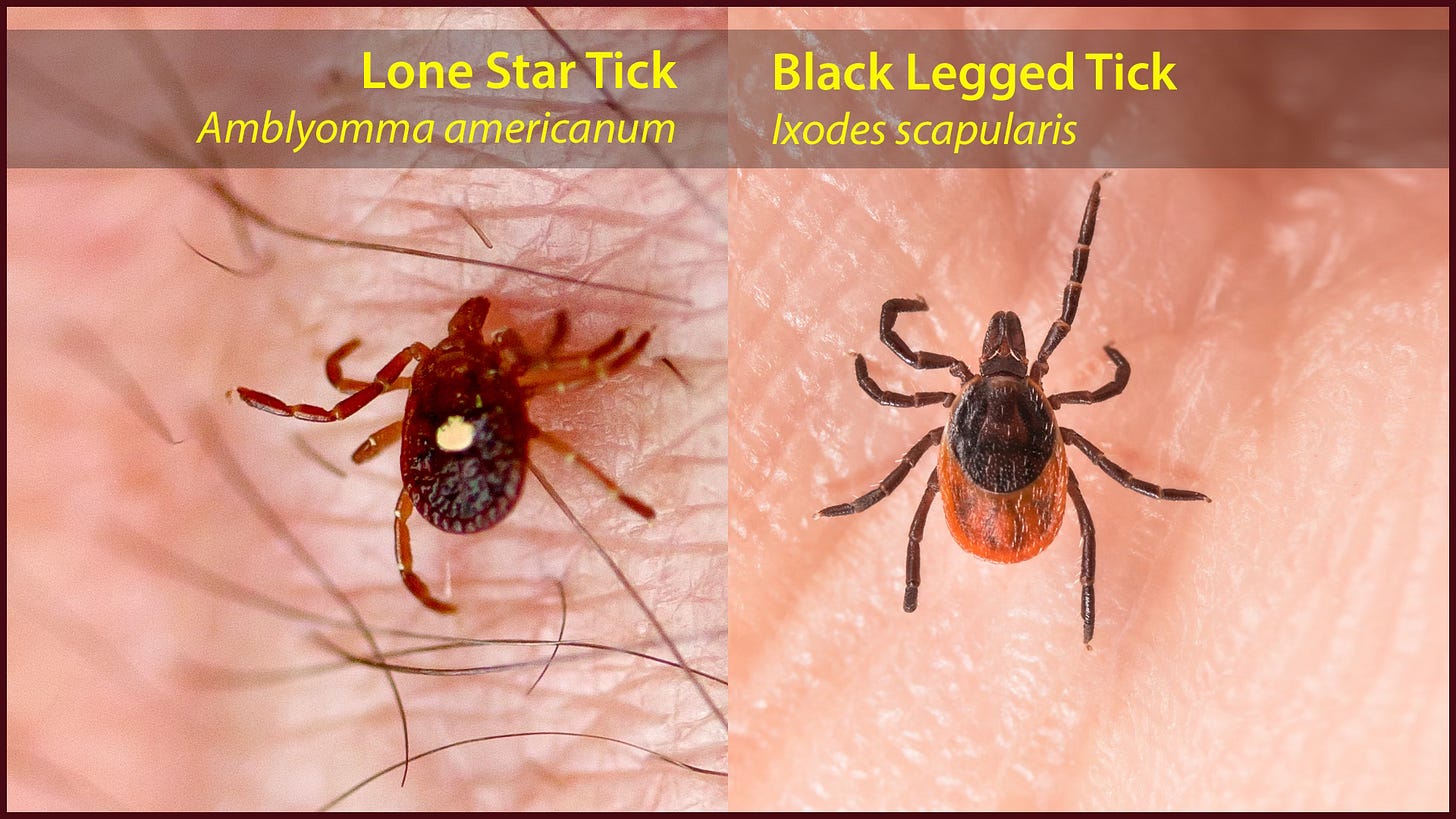
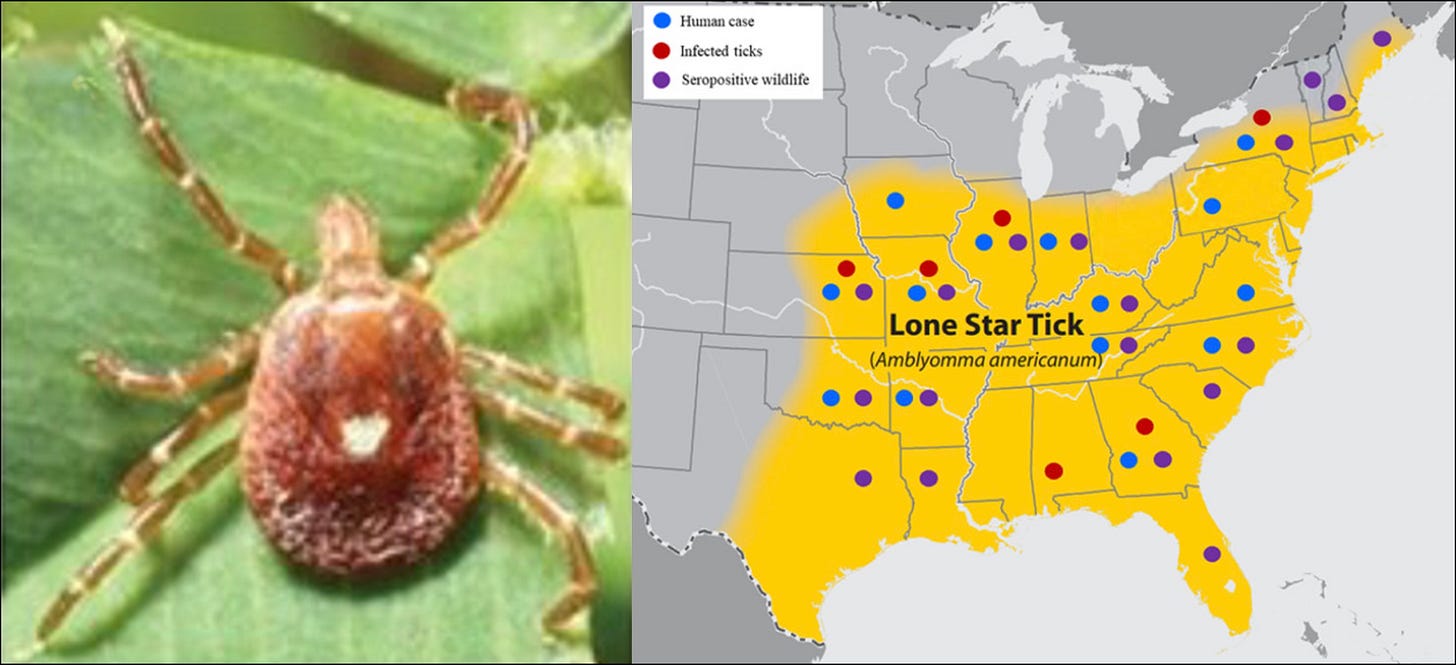
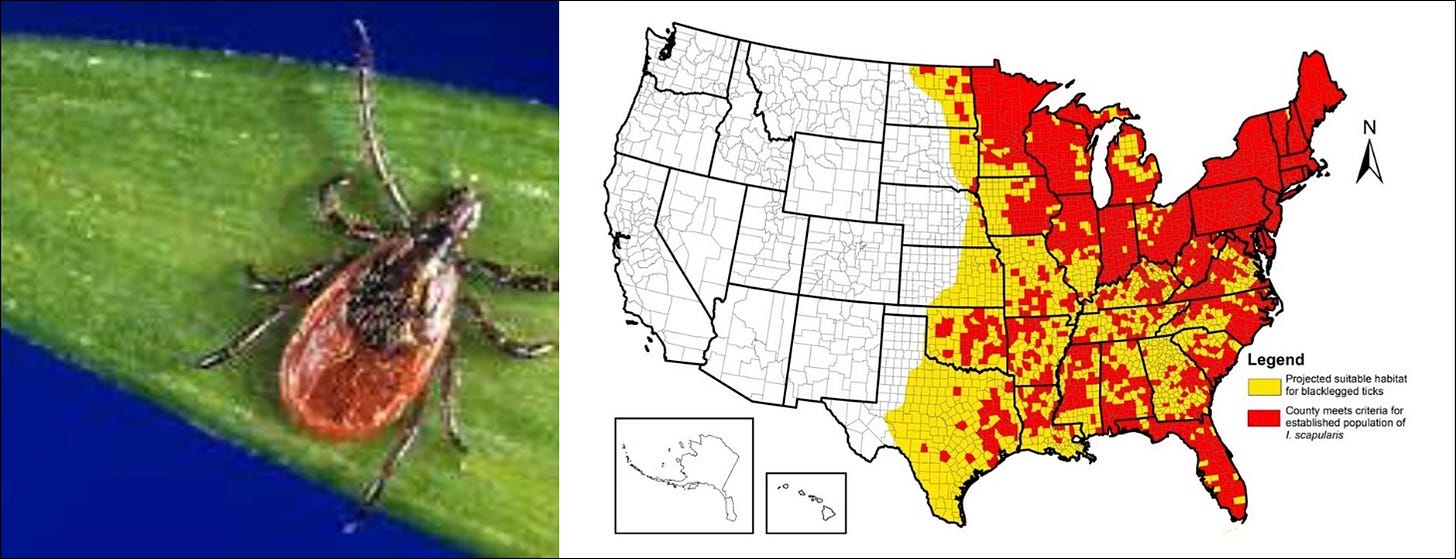
Ehrlichiosis refers to a group of diseases caused by the bacteria of the genus Ehrlichia. In the US, the most common species causing human ehrlichiosis are Ehrlichia chaffeensis, transmitted primarily by the Lone star tick (Amblyomma americanum, see above), and Ehrlichia ewingii, associated with the same tick vector. A less common but emerging pathogen is Ehrlichia muris eauclairensis, transmitted by the black legged tick Ixodes scapularis (see below). The incubation period for ehrlichiosis typically ranges from 1-2 weeks following an infected tick bite.
Symptoms of Ehrlichiosis
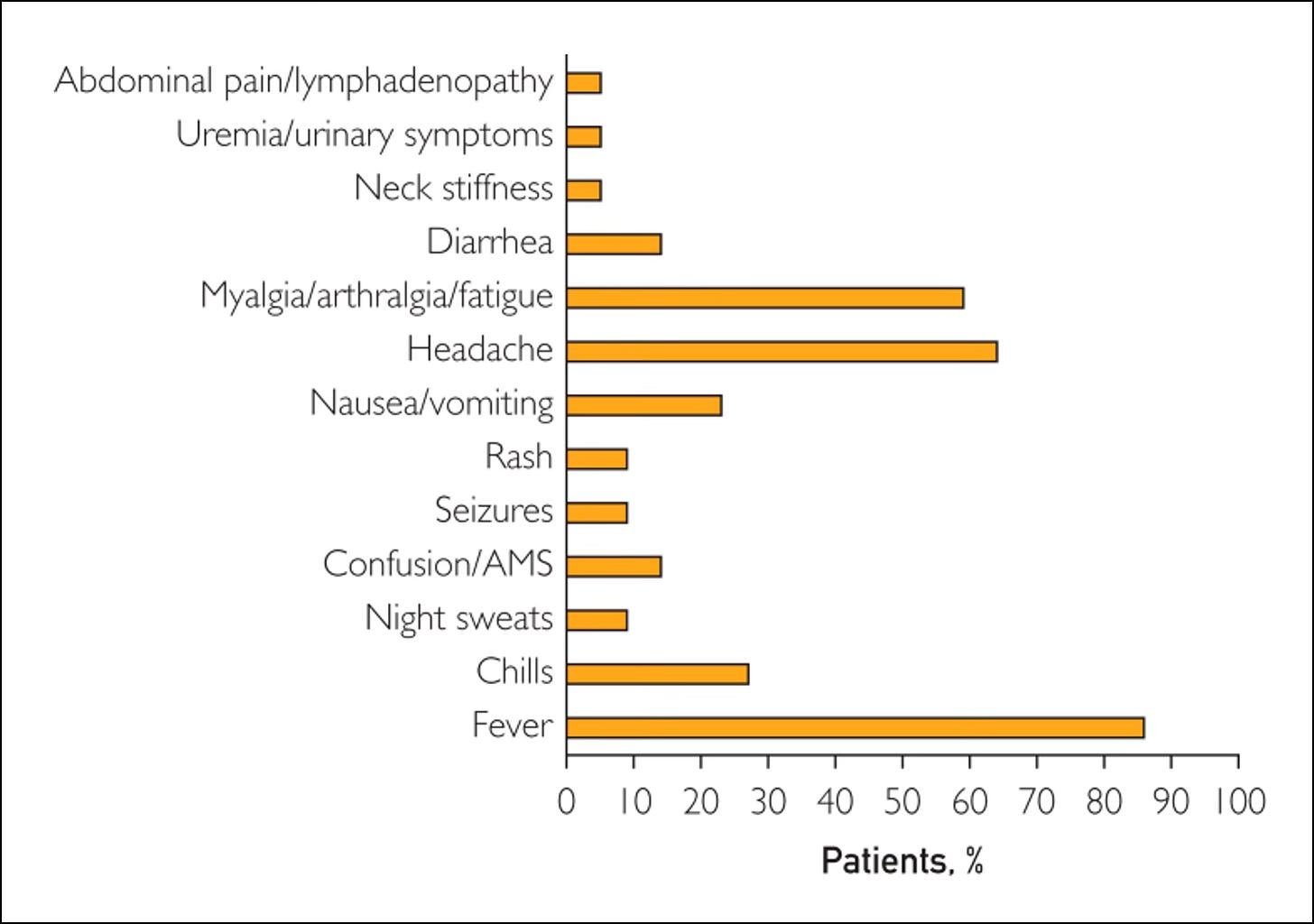
The onset of symptoms is often acute, characteristic of a flulike illness. Symptoms within the first 5 days usually include:
Fever: usually high, often reaching 102 to 104°F (39-40°C)
Shaking chills with night sweats (differential diagnosis includes Babesia!)
Severe headaches, often described as intense and persistent
Muscle aches and generalized body aches and pains
Gastrointestinal symptoms: nausea, vomiting, diarrhea and loss of appetite
Fatigue: severe and profound weakness
Central Nervous System: neck stiffness and confusion: altered mental status with disorientation, occasionally seizures
Rash: this occurs in up to one third of patients, more commonly in children with an Ehrlichia chaffeensis infection. The rash can be maculopapular (flat, red spots with small bumps) or petechial (tiny, pinpoint red or purple spots due bleeding under the skin). It typically appears around 5 days after the onset of fever.
In a study published by the Mayo Clinic in April 2025, these were the presenting symptoms:
If left untreated, Ehrlichiosis can progress to a more severe stage, potentially leading to life-threatening complications:
Damage to the brain or nervous system (Meningoencephalitis): inflammation of the brain and surrounding tissues, potentially causing neurological deficits, seizures or coma. Another reason to do regular tick checks and tick prevention!
Respiratory failure: difficulty breathing, requiring oxygen support
Uncontrolled bleeding due to decreased platelet counts or other coagulation abnormalities
Organ failure: dysfunction of vital organs such as the kidneys, liver, or lungs
Death: although rare with prompt treatment, severe ehrlichiosis can be fatal.
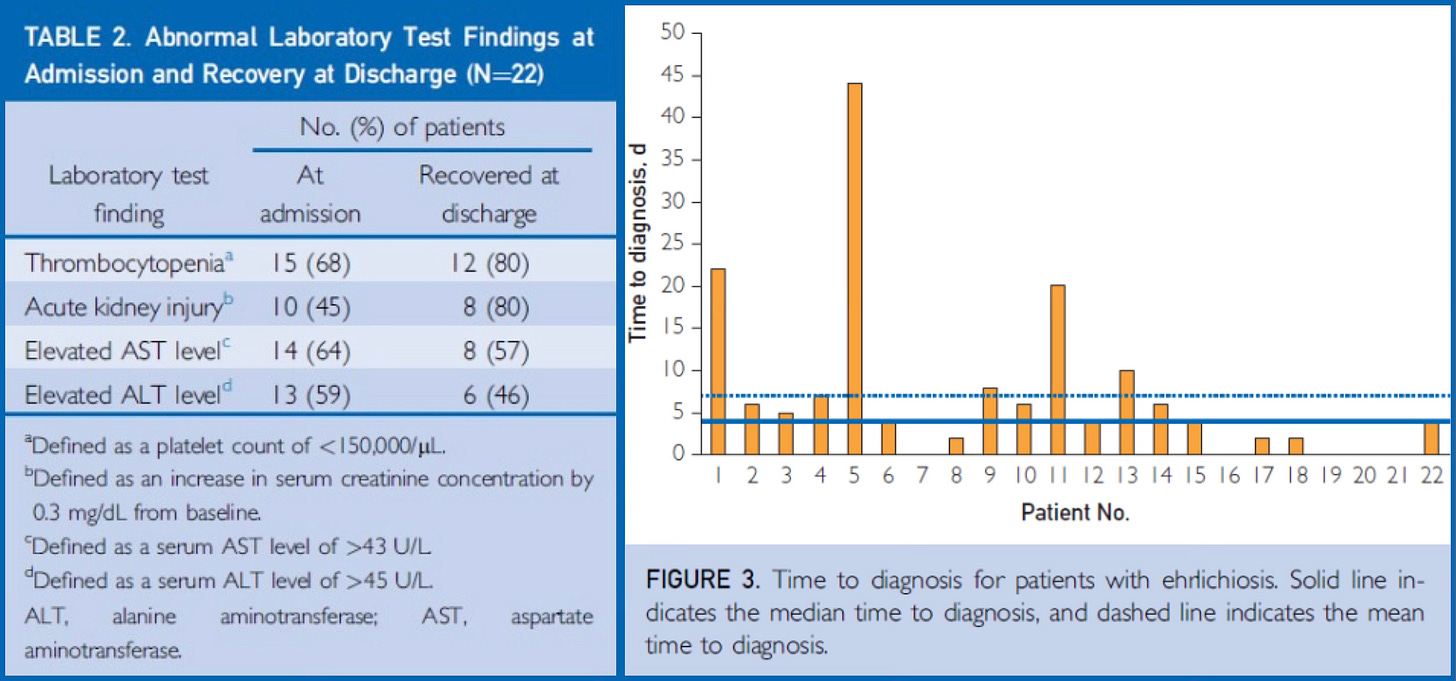
Diagnosing Ehrlichiosis
Diagnosing Ehrlichiosis can be challenging due to the nonspecific nature of early symptoms. A thorough history, including potential tick exposure and geographic location, is crucial. Laboratory tests play a vital role in confirming the diagnosis, but if there is a high level of clinical suspicion that you have been exposed, early antibiotic treatment is advised before blood tests return because of the potential for severe complications.
Blood Tests:
Complete Blood Count (CBC): low white cell counts (leukopenia) and/or low platelet counts may be seen early on in the illness
Elevated liver function testing: an increase in transaminases is common.
Kidney function abnormalities may be seen.
Indirect Immunofluorescent Assay (IFA): This serological test detects antibodies against Ehrlichia species. Paired samples taken during the acute and convalescent phases (2 to 4 weeks apart) showing a significant increase in antibody titers confirm the diagnosis. However, antibodies may not be detectable in the early stages of the illness, limiting its use for immediate diagnosis.
Polymerase Chain Reaction (PCR): This molecular test detects Ehrlichia DNA in blood samples and is most sensitive during the first week of illness. A positive PCR result provides rapid and specific identification.
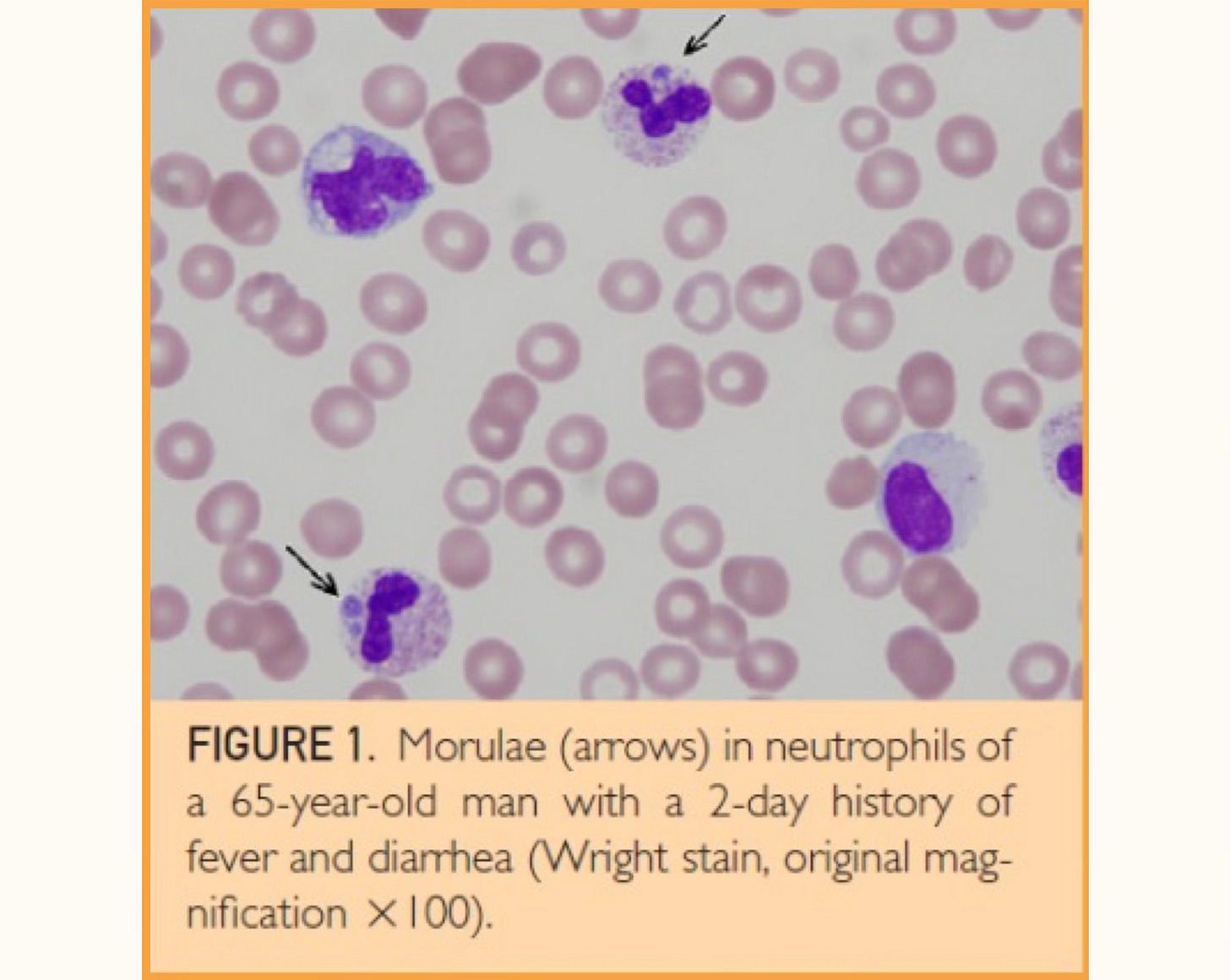
Wright-Stained Blood Smear: in some cases of Ehrlichia chaffeensis infection, characteristic clusters of bacteria called morulae can be visualized within monocytes (a type of white blood cell) on a blood smear. However, this method has low sensitivity.
Treating Ehrlichiosis
Prompt antibiotic treatment is essential for managing Ehrlichiosis and preventing severe complications. Doxycycline 100 mg 2x/day for a minimum of 7 days is the first-line treatment for adults and children of all ages with suspected or confirmed cases. It is highly effective, and early doxycycline treatment typically leads to rapid improvement in symptoms within 24-48 hours. The treatment should continue until at least 3 days after the fever subsides, and clinical improvement is observed. More severe cases may require treatment for 2-3 weeks. In the recent Mayo Clinic study, if there is a doxycycline allergy or contraindication, rifampin may be considered, although doxycycline is preferred due to its efficacy and safety profile. Older tetracyclines caused tooth staining in young children, like tetracycline hydrochloride, so doxycycline should not be withheld in children less than 8 years old or in a pregnant patient with known exposure due to potential complications.
A delay in treatment can increase the risk of severe illness and long-term sequelae. Symptoms can escalate rapidly, leading to acute kidney and liver failure, necessitating hospitalization. When that happens, in addition to antibiotics, complications such as respiratory distress, bleeding, or organ failure need to be treated with intravenous fluids, oxygen therapy, blood transfusions, or other interventions.
Anyone with sudden high fevers, shaking chills, severe headaches, and muscle aches WITH gastrointestinal symptoms of nausea, vomiting, and diarrhea and a rash, should not assume this is a viral infection. Get a CBC and CMP with liver and kidney functions done immediately. Any low white cell counts, low platelet counts, and/or elevated liver functions (a classic tickborne hematological triad) with renal involvement implies Ehrlichia may be present, and doxycycline should be taken immediately. Do NOT wait for antibody testing to return! Lack of response implies a parasite (like Babesia) or tick-borne virus.
You Don’t Want to Get Anaplasmosis
Anaplasmosis is a tickborne illness caused by the bacterium Anaplasma phagocytophilum. In the US, it is primarily transmitted by the black-legged tick, Ixodes scapularis in the Northeast and upper Midwest, and the Western black-legged tick, Ixodes pacificus on the Pacific Coast.
Symptoms of Anaplasmosis
The incubation period for Anaplasmosis is typically 1-2 weeks after an infected tick bite. Many people only have experience mild or even asymptomatic infections, while others develop a more pronounced illness. Symptoms often overlap those of Ehrlichiosis, and within the first 5 days usually include:
High fevers and shaking chills
Severe headaches are often a prominent symptom
Severe muscle aches can be quite debilitating
Gastrointestinal symptoms: nausea, vomiting, diarrhea, and loss of appetite
Extreme fatigue and weakness
A cough with shortness of breath can be seen in up to 1/3 of patients
Rash: this is uncommon in anaplasmosis and occurs in less than 10% of cases, and may suggest a co-infection with another tickborne pathogen like Borrelia burgdorferi.
Severe illness is less common with Anaplasmosis compared to Ehrlichiosis but can occur especially in older or immunocompromised individuals. The same types of complications can arise with respiratory failure, potentially requiring mechanical ventilation; bleeding and hemorrhage due to low platelet counts or other coagulation issues; organ failure of the kidneys or liver; and neurological involvement with a meningoencephalitis, focal paralysis, or other neurological complications. Even if severe complications are rare, you still need to be vigilant and consider early treatment if you think you have been exposed. Persistent intracellular bacterial infections including Anaplasma can also lead to exhaustion of T cells, immune-fighting cells needed to fight viruses (like Covid) and cancer.
Diagnosing Anaplasmosis
Similar to Ehrlichiosis, the diagnosis of Anaplasmosis relies on a combination of clinical suspicion and laboratory testing:
Complete Blood Count (CBC): often reveals low white cell counts (leukopenia), and low platelet counts (thrombocytopenia)
Liver Function Tests: elevated liver enzymes (transaminases) are frequently observed.
Peripheral Blood Smear: in some cases, as with Ehrlichia, morulae (clusters of bacteria) can be seen within neutrophils, another type of white blood cell on a Wright-stained Blood smear, although this method has limited sensitivity.
Polymerase Chain Reaction (PCR): PCR testing is highly sensitive and specific for detecting Anaplasma phagocytophilum DNA especially during the first week of illness
Serology (IFA): Antibody testing using IFA and confirm the diagnosis, particularly with paired acute and convalescent sera showing a significant rise in antibody titers. However, like Ehrlichiosis, seroconversion may take one to 2 weeks making it less useful for early diagnosis when treatment is essential.
Treating Anaplasmosis
Prompt antibiotic treatment with doxycycline is crucial for Anaplasmosis to prevent severe outcomes. Typical treatment lasts 7-10 days, or at least 3 days after the fever resolves and clinical improvement is seen. Early treatment with doxycycline usually leads to rapid clinical improvement within 24 to 48 hours. As with Ehrlichiosis, treatment should be initiated as soon as the diagnosis is suspected, even before lab results are available. In cases of doxycycline allergy or contraindication, rifampin may be considered, although again, its efficacy is less well established.
For severe cases without prompt treatment, hospitalization will be needed to manage complications including respiratory distress, bleeding, or organ dysfunction.
You Don’t Ever Want to Get a Tick Bite! Prevention Is Crucial
The ticks are out in full force this spring. New York Tick Control (1-888-NIX-TICKS) sprays our property twice a year and has been doing so for over a decade. They have installed 50 bait boxes around our property, yet we still will find an occasional tick on our dog Mali if she strays beyond our property lines or if we take a walk in local state parks, even trying to stay on paved paths. Many of my patients have called the office this year letting me know of tick bites; they needed immediate prophylactic doxycycline.
Before you go outside, always remember to wear permethrin-treated clothing. You can either buy clothing embedded with permethrin or take clothing outside and spray it (not while you are wearing it). Let it dry for 4 hours, and it is good for several washings. Permethrin will kill ticks.
For skin protection, I use picaridin 20% on my skin as I find the higher dosage is also more effective for mosquitoes (I have tried 5% and 10% and they still love me). Lemon eucalyptus oil and IR 3035 (Avon SSS) are also potential options. IR 3535 is an amino acid base and has been shown to be safe in pregnancy.
Be vigilant! Do tick checks when you come inside. Take a shower and check yourself and consider throwing your clothes in the dryer at high heat for 10 minutes, which will kill any ticks on them.
A tick bite can make you really sick. Stay safe this spring!