Babesia – A Long and Tortuous Medical Journey to Find Treatment Options in a Highly Resistant Patient: Part 3 of 3
Lao Tzu, the famous Chinese philosopher, once said, “The journey of a thousand miles begins with a single step.” In my case, the Jewish Zen philosopher’s quote, which made me laugh out loud when I read it in David M. Bader’s book, Zen Judaism, is more appropriate: “The journey of a thousand miles begins with a single Oy.”
Drug-Drug Interactions Are a Potential Concern with Most Babesia Regimens
It has been a long and tortuous journey to get the answers to Babesia. When I started finding and treating it for the first time in the 1990s, there were very few choices available to give patients. Clindamycin plus quinine was the standard treatment and there wasn’t much else available. Although the treatment was generally effective, the side effects made you question whether the illness or the treatment was worse. Quinine caused nausea, vomiting, occasionally a rash, and severe ringing in the ears (tinnitus) that made it sound like an alarm clock was next to your head 24/7. Clindamycin required very high dose probiotics because of the risk of antibiotic-associated diarrhea like Clostridium difficile. So, in the worst-case scenario, you would be deaf with diarrhea while trying to cure this illness. This regimen was so difficult that I often had to joke with my patients to assure them that I really did like them and was not torturing them on purpose. My standard joke with those suffering from quinine-induced hearing problems was to make believe I was talking to them with no words coming out of my mouth. Some found it funny; others did not (with those patients, I had to assure them that I was not running the Marquis de Sade medical clinic!).
Then there was the problem of drug-drug interactions, since quinine could affect the heartbeat, causing a prolongation of the QT interval (an important electrical signal on the EKG); in rare cases, this could result in fatal cardiac arrythmias and death.
Yes, this was the best medicine had to offer for Babesia treatment in the 1990’s! I had to check the electronic PDR (Physicians’ Desk Reference) before administering these medications to ensure it was safe to mix quinine with other drugs, and had to get a baseline EKG beforehand to ensure that I wouldn’t kill my patients. I had to be careful mixing quinine with a broad range of prescription drugs including macrolides (Zithromax, Biaxin), quinolones (Cipro, Levaquin), Coartem (lumefantrine/artemether), mefloquine (Lariam), proton pump inhibitors like omeprazole or Nexium, antidepressants in the SSRI class (i.e., Prozac), or amitriptyline (Elavil). Then once I started this 7-10-day torturous regimen to reduce my patient’s day and night sweats, shaking chills, flushing, cough and air hunger (shortness of breath) from Babesia, I had to repeat the baseline EKG to ensure that what I was doing was safe. Although some patients got through it and did get better, some begged me to stop it, as the side effects were so bad. They told me that the treatment was worse than the illness itself. Back to the drawing board.
The Discovery of Babesia in Ticks and My Patients in the Late 1990s
In the late 1990s, I discovered atovaquone (Mepron) and azithromycin (Zithromax) for the treatment of Babesiosis. After a conversation with Dr. Joe Burrascano about Babesia--and since the drug atovaquone had been used in other parasitic infections like PCP (Pneumocystis carinii pneumonia), which we had been seeing in HIV patients--we decided to try it. He encouraged me to publish my findings (thank you, Joe!) after we found it to be effective.
We went looking for Babesia microti in both ticks and in my patients, and one of my wheelchair-bound patients began to walk for the first time in 5 years (!) after only 10 days of taking Mepron and Zithromax. I then realized the power of Babesia to adversely affect my patients’ health.
Some of the abstracts that I published on Babesia at the 11th, 12th, and 13th International Lyme conferences are listed below. Keep in mind, these are 25 years old, and will be important when I explain where we are now with Babesia testing and therapeutics a quarter-century later.
We first had to prove that Babesia existed in our area, in both ticks and patients. We contacted Dr. Rick Ostfeld from the Institute for Ecosystems Studies in Millbrook, NY, thanks to one of my patients, and got 30 ticks from our area to send out for analysis. This was the result:
We proved with this initial study that Babesia was in my area of the Hudson Valley, NY, and when my patients were presenting with drenching sweats and chills, the Medical Detective in me had to rule out overlapping causes and prove that Babesia was in fact the only reason why this was happening. I tested and ruled out hyperthyroidism, menopause, malaria, tuberculosis, non-Hodgkins lymphoma, or other bacteria known to cause high fevers and drenching sweats like Q-fever (Coxiella burnetti) or brucellosis. When men would come in with these drenching sweats, I would ask them if they suffered from “manopause.” Depending on how bad their cognitive dysfunction was from Lyme disease, they either got the joke, or didn’t. If they didn’t, I knew more treatment was needed.
After finding Babesia in both ticks and patients, and because Clindamycin plus Quinine was so poorly tolerated, we did a more extensive study on atovaquone and azithromycin to see if we could find a more effective and easier protocol. Here is the initial abstract:
We published this abstract over 2 years before Dr. Peter Krause published his landmark article in the New England Journal of Medicine in 2000 on using this regimen for the treatment of Babesiosis. Sounds good, right?
You might think that with such incredible results, my local medical community would have been as excited as I was to have found a new treatment helping wheelchair-bound people walk. Many patients who had not improved after standard Lyme treatment were getting better. But, it turns out, I was quite naïve. I brought in the local health department and HMOs to demonstrate my findings, since this was the first time Babesia had been found in the lower Hudson Valley, and the parasite was known to be a significant risk for illness and even death in the very young, elderly, and immunocompromised. I wanted to make sure that I shared my findings with the scientific community, since if my patients were testing positive, others surely were as well, and it could be a significant health risk for our community. After all, my job as a doctor is to help people!
Despite finding it, with positive Babesia titers, smears, and PCR (polymerase chain reaction, a DNA test) in 120 of my sick patients--which is not a small number--I was told by the powers-that-be that “this parasite could not possibly exist where we lived, and that these were false positive results.” Try telling that to my patient who walked out of a wheelchair after 5 years of disability! I was subsequently thrown out of my HMO and an insurance company for using “expensive drugs for an illness that did not exist.” Then I had to go before the medical boards to explain why what I was doing was in fact correct and based in science. Wow. I instantly lost up to 2,000 patients because of my problems with insurers, and had to remortgage my house to keep our medical practice open. I could no longer take insurance, because they didn’t want me. FYI, during this time, I was also regularly fighting with the head of the HMO who told me to follow IDSA guidelines, and that I should not be using more than several weeks of antibiotics for Lyme disease because it wasn’t a persistent bacteria…yet my patients were responding to this treatment and getting significantly better.
That was when the rubber met the road, and my ethics and morality in medicine told me that I had to put patients first, not insurance companies. I remembered once more what my spiritual teacher, Lama Guendun Rinpoche, told me when I was leaving medical school: “Put yourself in your patient’s shoes and do for them what you would want done for yourself, and everything will go well.” Spiritual test number one. Check. Not easy.
That was my first taste of the dysfunctional politics of Lyme and associated co-infections. I had walked onto a medical-political battlefield without ever realizing there was a war going on. But it didn’t stop me from continuing to look for answers--and several years later, the NY State Department of Health confirmed that Babesia microti did in fact exist in the lower Hudson Valley…I work for them now. Although Mepron and Zithromax were helpful, and better tolerated than Clindamycin and Quinine, we still found Babesia persisted in many of our patients despite these two regimens.
In April 1999, I presented an abstract at the 12thInternational Scientific Conference on Spirochetal and Tick-borne Disorders, showing that the parasite persisted despite both regimens:
I then went on to look for other treatments since some patients continued to have symptoms and positive testing for Babesia, and I started to publish on the importance of co-infections in my patients with Lyme:
Chronic Lyme Disease: A Symptom Complex of Multiple Co-Infections: New Diagnostic & Treatment Protocols. Horowitz, R.I., M.D. 12th International Conference on Lyme Disease and Other Spirochetal and Tick-Borne Disorders, April 9-10, 1999. New York, New York.
Lyme Disease and Babesiosis: New Therapeutic Options for Chronic Persistent Disease. Horowitz R.I., M.D.. Abstract, 13th Annual International Scientific Conference on Lyme Disease and other Tick-Borne Disorders. Hartford, Connecticut, March 25-26,2000.
Mefloquine: The Next Treatment for Resistant Babesia
One of the next treatments I tried was with a different drug, used to treat and prevent malaria, called mefloquine (Lariam). This is the abstract:
Mefloquine and Artemesia: A Prospective Trial of Combination Therapy in Chronic Babesiosis Horowitz R.I., M.D. Abstract, 13th Annual International Scientific Conference on Lyme Disease and other Tick-Borne Disorders. Hartford, Connecticut, March 25-26, 2000.
It did help some patients who had failed the 2 traditional protocols, but we had to carefully ensure that these patients were psychiatrically stable. We also had to watch QT intervals again, as Lariam has a very long half-life, and it causes nausea and dizziness when administered with a typical loading dose of 5 pills all at once. I was at a stage in my medical career where I felt that I should know what my patients were going through, so I took the 5-pill dose myself to see how bad it was (not sure what made me think I had to do this). It reminded me of researchers like Dr. Trevor Marshall, who discovered that H. pylori was the cause of stomach ulcers by taking a drink with the bacteria to prove his point. Well, I didn’t give myself Babesia (I was not going to go searching for ticks!), but after taking the 5 pills all at once and collapsing into bed with dizziness for 2 days, I decided to stop that dose in my patients and extend the treatment over several days. That is one way to develop compassion in medicine! Lower doses did help decrease the side effects, and I was able to commiserate with my patients. Eventually, I learned I could just use half a pill twice a week and add artemisinin, a Chinese herb, 3 times a day, along with doxycycline 100 mg twice a day, and have some improvement in malarial-like symptoms. There was a 21.5% improvement in overall symptoms, but I had to monitor any neuropsychiatric effects (transient depression and anxiety). Still, roughly 22% of my patients continued to be positive by DNA (PCR) testing despite the treatment. This regimen was helpful, but I rarely use it now. I needed to go back to the drawing board to see if I could find something more efficacious and better tolerated.
Next Step: A Trial of High-Dose Bactrim (Trimethoprim-Sulfamethoxazole) at the HVHAC
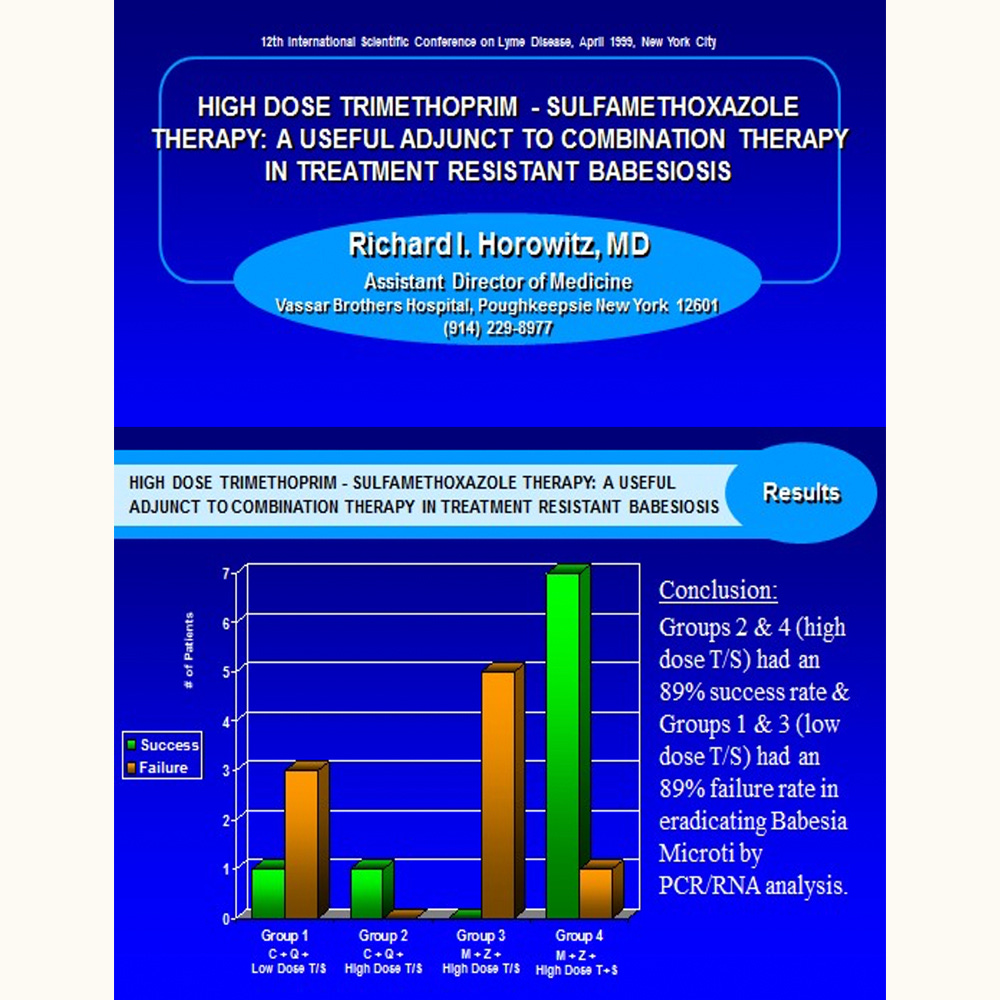
I went back to the medical literature and looked for other options, and in 1995 I found a promising article in the American Journal of Hematology. Gupta et al. reported that when he used high-dose trimethroprim-sulfamethoxazole in addition to Clindamycin, quinine and Atovaquone, parasites in the blood (parasitemia) improved. I decided to try it in 2 groups, where we added lower dose Bactrim DS, one 4x per day (QID) or 2, 4x per day to patients taking standard Babesiaprotocols, like Clindamycin/quinine or Mepron/Zithromax. Here are the results:
The regimen was helpful, and it demonstrated that high doses of sulfa drugs like Bactrim DS had a positive effect on treating Babesiosis due to B. microti with an 89% success rate. However, the side effects of nausea and vomiting using high-dose Bactrim made it difficult to tolerate in some patients. They needed anti-nausea drugs, and there are limited options; Zofran (ondansetron) is helpful at 8 mg 3x a day, but can also cause QT prolongation, so repeat EKGs are necessary when using it in combination therapies with other QT-prolonging drugs.
We were making progress, and this study was foreshadowing the success I would have almost 20 years later with another sulfa drug, dapsone, for the treatment of chronic Lyme disease and Babesia. In 2016, we published our first landmark study on the use of dapsone combination therapy for the treatment of chronic Lyme disease (Horowitz, Freeman, J Clin Exp Dermatol Res 2016, 7:3). We’d found that this sulfa drug also had an effect on malarial-like symptoms seen in Babesiosis. Those who had moderate, moderately severe, or severe Babesia symptoms noticed the most improvement.
Yet, despite dapsone’s efficacy--and the efficacy of the only other sulfa persister drug to be published in the medical literature for the treatment of chronic Lyme disease (disulfiram), which also helped to knock down Babesia symptoms--these newer treatments were often not enough to completely eliminate the parasite. Back to the medical literature….
Trials of Coartem (lumefantrine/artemether), Malarone (atovaquone/proguanil), Alinia (Nitazoxanide), and Herbal Protocols
Let me speed up this journey through my life as a Lyme doctor, scientific researcher, and Medical Detective and simply say that I am not one to give up—in case you haven’t yet noticed...!
I kept on going back to the medical literature, trying other anti-malarial medications and herbal protocols over the years. They were helpful. Coartem (lumefantrine/artemether) at a dose of 4 tablets, twice a day, 3 days in a row, every 2 weeks (3 days on, 11 days off) definitely knocked down Babesia symptoms in my patients but was not necessarily curative. Since this drug also could prolong QT intervals, the same precautions were needed, as above. We also tried Malarone, a pill form of Mepron (atovaquone) and published several studies in the medical literature that it could be helpful in decreasing Babesia symptoms and sometimes mixed it with Coartem. We used higher doses of Malarone (4 a day) for months on end, mixed with different herbs (it can’t be mixed with CoQ 10, which can interfere with the efficacy of the atovaquone). Again, it was helpful, but not curative. Some patients had overlapping parasitic infections in their gastrointestinal tract, like Giardia or cryptosporidium, and when we gave them Alinia (nitazoxanide) for 3-5 days, a different anti-parasitic medication, it seemed to have a partial effect and help lower the load of the Babesia parasite, helping symptoms. But we had difficulty eliminating these gastrointestinal parasites completely, despite rotations of different anti-parasitic drugs.
We found out later on that an infection with Babesia interferes with your immune system’s ability to clear other parasites from the body. This is one tricky bug. And then the medical literature finally explained why we were having such problems clearing the parasite. B. microti ended up having genetic mutations making it more resistant to standard therapies, and B. duncani also had an unusually high tolerance to recommended therapies.
These studies on the resistance of Babesia to standard therapies were published almost 20 years after I presented my research at the International Lyme conferences, discussing how resistant this parasite was! Wheels turn slowly in medicine. But now we had more scientific evidence showing why we were having such trouble completely eliminating the parasite from the body.
Enter Herbal Therapies for Babesia
Johns Hopkins researchers, along with Dr. Sunja Schweig and colleagues, subsequently published an article on botanical medicines that showed they could be helpful for treating Babesia duncani. The 5 we regularly use now, in combination with our other therapies are:
Cryptolepis sanguinolenta (Cryptoplus, Researched Nutritionals) 30 drops 3x a day
Artemisia annua (Dr Zhang, Traditional Chinese medicine) one 3x a day
Scutellaria baicalensis (Chinese Skullcap)
Polygonum cuspidatum (Japanese knotweed)
Alchornea cordifolia.
These last 3 can be obtained in liquid form, used 3 times a day, to decrease the number of capsules, and can be obtained online from Green Dragon Botanicals or Woodland Essence.
It also turns out that methylene blue, the compounded medication that we use as a persister drug to treat chronic Lyme (which lowers methemoglobin levels, a side effect of dapsone where you don’t carry oxygen well in the blood), also has some anti-malarial properties. It can be useful in combination therapies in helping to decrease Babesia symptoms. But despite all of these treatments, there are still patients who suffer from chronic Babesiosis. Enter the last treatment to be published for Babesia: tafenoquine.
Tafenoquine and Atovaquone for Resistant Babesia
We have finally arrived at the last treatment that has been published in the medical literature for resistant Babesiosis. It was published in 2024, and involves using an anti-malarial drug, tafenoquine, 100 mg tablets, 2 a day, for 3 days in a row (600 mg loading dose), followed by 200 mg (or 300 mg) once a week of tafenoquine, taken along with atovaquone 750 mg twice a day for 6 weeks (the lower doses do not clear Babesia microti as well in our patients, so we often use 1500 mg of atovaquone twice a day, and higher doses of weekly tafenoquine, i.e., 300 mg, as it has been shown to improve the clearance of B. microti). This regimen has helped to put some of my chronically ill Babesia patients in remission. But because of how resistant this parasite is, we often use azithromycin, and ivermectin (0.2 mg/kg once a day) with atovaquone, as well as the 5 herbal therapies listed above.
The Side Effects of Tafenoquine
Tafenoquine has two potential side effects that are important to know about. The first is hemolytic anemia, where blood cells can burst apart, causing some decreases in red cell counts (but not as significant as seen in dapsone combination therapy). The other side effect is an elevation in methemoglobin, similar to what can happen during dapsone therapy. You need to have the enzyme G6PD (like with dapsone) before taking this medication. Also, the medication can have some adverse psychiatric effects (suicidality, psychosis) similar to its cousin, mefloquine (it also can potentially cause dizziness and vertigo), although we have not seen that to date with our patients. A Physicians Desk Reference should be consulted for the full range of potential side effects. The medicine is contraindicated in pregnancy (as many are), and due to elevated methemoglobin levels, dapsone should not generally be given at the same time as tafenoquine. We suggest using a similar protocol we use in dapsone combination therapy to help lower methemoglobin when using tafenoquine: high dose glutathione, at least 1000 mg twice a day, vitamin C (1 gram twice a day), vitamin E (300 IU twice a day), cimetidine 400 mg BID, and Methylene Blue, at least 100 mg twice a day (levels of methemoglobin need to be checked).
This regimen has definitely helped some patients with resistant Babesiosis, but it has not been uniformly effective. Other treatments like orlistat (a weight loss drug that has some potential to treat B. duncani) and an ACE inhibitor like fosinopril (normally used for high blood pressure) have been discussed in the medical literature as having potential promise for Babesia, but more work is required in this field to find better therapies. However, rotations of the above medications and herbs—coupled with not giving up--eventually does seem to knock down the load of Babesia over time so patients can feel better.
And If Nothing Else Works, Take Out the Bad, Put in the Good: Exchange Transfusion
During an exchange transfusion, your blood is replaced with fresh blood from a donor. This is a last resort for very sick, hospitalized patients with high levels of the parasite in their blood, who are failing the above protocols. It is also sometimes needed to treat critically ill individuals.
Knowing About Babesia Is Critical to Your Health
Now that we have shared this tortuous (and torturous) journey together, I would like to end this Medical Detective Substack with a quote again from the book Jewish Zen, which seems particularly appropriate considering what you’ve just read: “Accept misfortune as a blessing. Do not wish for perfect health, or a life without problems. What would you talk about?”
Please feel free to share this and the previous 2 Medical Detective Substacks on Babesia with those you care about. Just make sure when you talk to them about this parasite, you spell it out clearly. After telling one of my patients about Babesia, she decided to look it up online and came back to me incensed. “Dr Horowitz, how could you send me to that gross website?” she asked. “What do you mean?” I said. “I looked up what you told me,” she replied. “It sent me to an Asian porno site, ‘Babes in Asia.’”
I couldn’t make any of this up if I tried!