Everyone’s Wrong About the United Healthcare Murder: We’re All Victims of Our Broken Healthcare System
*Note: I had intended to run all 5 of the Meditation Substacks in a row, but this situation is so vitally important to discuss that I wanted to share my thoughts with you now. This will be next week’s Substack, published early…
The recent tragedy and murder of a healthcare executive has sparked a broad range of emotions and responses amongst the American public, ranging from the mainstream media lauding the head of United Healthcare (UHC) for his work empowering health, sustainability, and quality improvement, to people now being given a megaphone to yell out their frustrations with insurance companies, especially the frequent denial of essential health care, with some on social media lauding the shooter as a folk hero.
This situation reminds me of Network, chosen by the American Film Institute as among the 100 greatest American Films of all time, winning 4 Oscars after its release in 1976. If you haven’t seen it, or even if you have, I suggest watching it again. It is one of my favorite films of all time. It had an incredibly prescient look at our society and media, sarcastically illustrating how we influence people’s lives through propaganda coming through our social media channels (in those days, television sets, now cable media outlets, TikTok, etc.). In the movie, people were upset about the economy. They were out of work. Banks were going broke. There were wars and problems with Russia. The air was unfit to breathe, and food unfit to eat. Things were bad and crazy, and people were frustrated. Sound familiar? The most famous line in Network, which premiered almost 50 years ago, encapsulates the feeling of many Americans today. When a media executive, played by Peter Finch, went crazy on live national television, he didn’t shoot himself, or anyone else. Instead, he opened the window and shouted out: “I’m mad as hell, and I’m not going to take this anymore!” He encouraged people to go to their windows, open them up, and yell out their frustrations and anger. And people did. All over the country. They got mad.
Here is the movie clip from Network and its “Mad Prophet of the Airwaves,” reflecting the pent-up emotions and rage millions were feeling:
When it comes to our healthcare system, many people are now mad as hell and don’t want to take this anymore—especially when they desperately need essential care and it gets denied.
I experienced the inequities with our healthcare system when I was the first doctor to diagnose Babesiosis in upstate NY in the 1990s. I had people coming in with malarial-like symptoms, including drenching night sweats. After doing a differential diagnostic work-up, ruling out things like menopause, hyperthyroidism, malaria, Brucella, and other infections, I found Babesia in my patients, as well as in our local ticks, and gave them the accepted treatment, Mepron and Zithromax. Well, despite people in wheelchairs walking for the first time in 5 years, and many individuals getting their health back, the health department and insurers told me: “There is no Babesia in Dutchess County” and “the lab must be bad” (it wasn’t just IgeneX BTW, it was Labcorp, Quest, and MDL Laboratory with hundreds of positive PCRs in patients’ blood tests, definitive evidence by most lab standards). They told me outright that the cost of treatment was the main reason they were dropping me (I cost them over $70,000 in treatments), and I was “uninvited” to stay in insurance panels by two insurers, losing around 2,000 patients over 6 months. This forced me to almost close my medical practice and stop accepting insurance. I had to remortgage my house to keep my medical practice open, and it wasn’t until years later that the NY State Department of Health admitted that I was right and that Babesia did exist in our area.
During that time, how many hundreds or thousands of patients suffered from a treatable disease, which was denied for financial reasons? Insurers had clear evidence of a disease making people sick, yet they denied its existence. This is only one example, which impacted me and my patients directly. Denials in medical care are the rule, not the exception.
Of course, shooting a healthcare executive is not acceptable by any societal norms, even if we are frustrated with the system. We should have compassion for both this insurance executive and his family, as well as the pain and suffering of the man who is now arraigned on charges, and the pain and suffering his family is going through.
While the mainstream media is finally sharing horror stories about our broken healthcare system and how desperately it needs to be fixed, trying to make the point that was a cry for change, although fatally misguided, they are missing another point entirely.
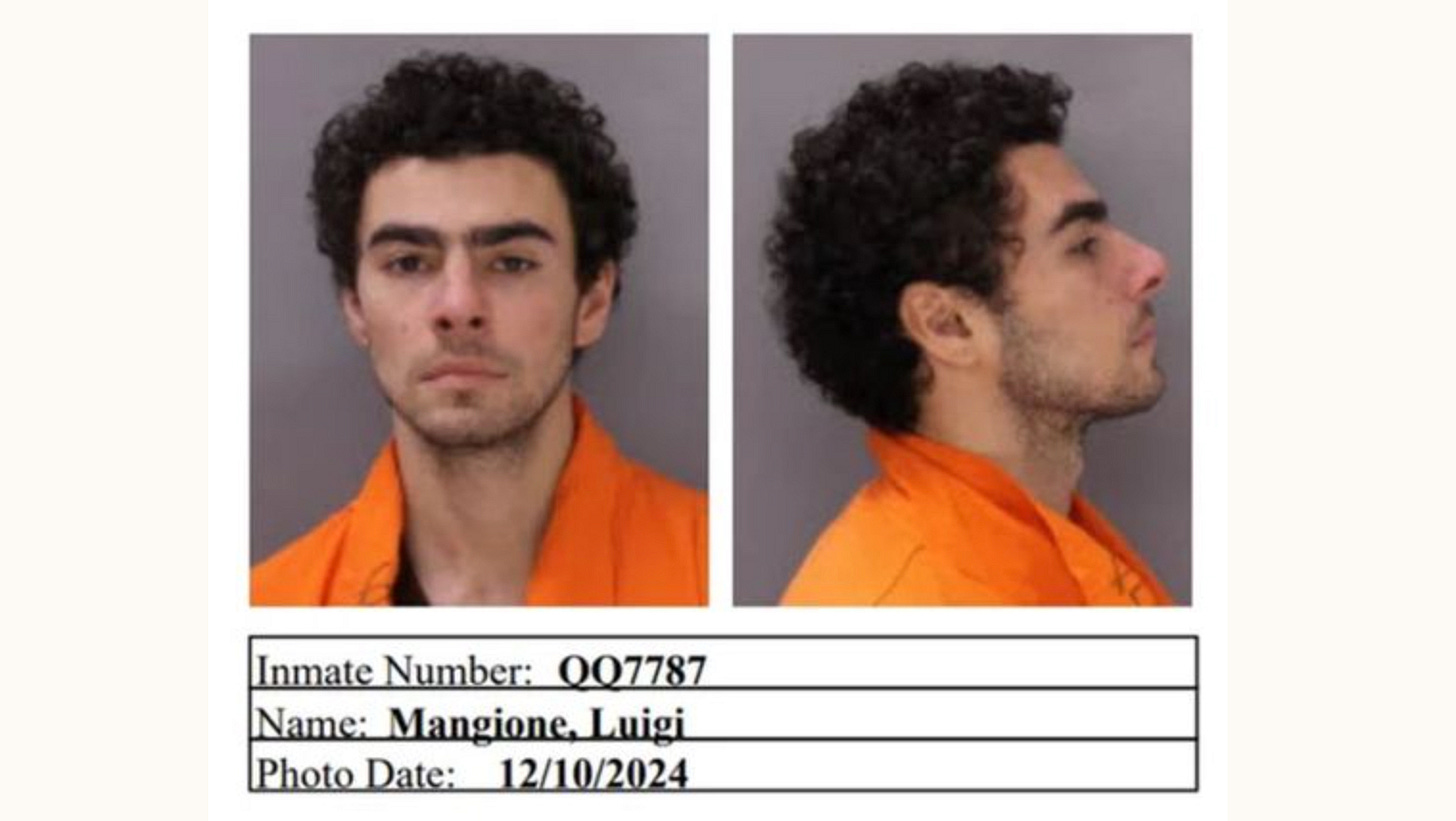
The shooter, Luigi Mangioni, had a recent history of back surgery and unrelenting, unbearable back pain. But no one in the mainstream/legacy media—has mentioned his history of Lyme disease.
Mangioni had complained of chronic brain fog and pain in the past. Chronic Lyme disease and associated co-infections can be associated with not just fatigue, pain and brain fog, but serious mental health issues. Chronic pain alone can cause mental health challenges and depression, but chronic Lyme has been associated with a broad range of psychiatric conditions, including homicidal tendencies. And we have seen underlying Lyme disease worsen surgical outcomes, from ongoing inflammation in the body.
As “Mister Cactus,” his posts quoted on Reddit after the shooting referenced health battles with Lyme disease as a teenager and the “brain fog” that accompanied it. “He missed soccer tryouts when he contracted Lyme at 13 and didn’t make the team, then started noticing ‘mild cognitive decline’ when he was 15, he posted. He said his symptoms severely worsened in 2017, when he was a student at the University of Pennsylvania, but additional tests for Lyme disease were negative. In July 2018 he posted about having restless sleep and in August that year he posted in a group about irritable bowel syndrome, asking for advice about a change in diet to improve his condition.”
Can chronic Lyme disease cause homicidal tendencies? Yes, and they can be worsened by co-infections like Bartonella and Babesia. Aggressiveness, violence, homicidality, and homicide have all been associated with chronic Lyme disease in the published peer-reviewed medical literature. *
I can’t say for sure whether Lyme and associated co-infections played a role in Mangioni’s psychiatric symptoms, along with his chronic pain influencing his mental health status, as I don’t intimately know the case, but nevertheless, it is a distinct possibility, especially knowing that this scenario has been published in the medical literature. And because of the controversies and political nature of chronic Lyme disease, where patients have been denied care by their physicians and insurers--who refuse to admit that it is a chronic, persistent infection despite hundreds of articles proving it--medical controversy involving insurers may be relevant here, as it could have impacted Mangioni’s physical and mental health.
Also, since he lived and went to school in Pennsylvania, which has had the highest incidence of Lyme disease in the country in 11 of the past 12 years, he could have been re-bitten, increasing his chronic pain and affecting his psychiatric symptoms. The majority of the patients I have seen from PA also have had Bartonella. According to a 2020 study of deer ticks in Pike County, Pennsylvania, 18.5% of the ticks tested positive for Bartonella species. Now we still are debating whether Bartonella is transmitted by ticks, as only one European study to date proved it in Ixodes ricinus ticks, but nevertheless, the majority of my sick patients now have Bartonella, and it significantly worsens neuropsychiatric symptoms, as well as fatigue, brain fog and pain. *
Please understand that this is all conjecture and is not intended to be an excuse for a horrible act of violence, but we have to account for all possible causes. America is plagued by epidemics of violence and unregulated guns, and we are plagued by an epidemic of Lyme and tick-borne disorders. Chronic tick-borne disorders, especially Lyme and Bartonella, can and do cause psychiatric symptoms, which can be severe. It is incumbent on the healthcare system to test him for Lyme and Bartonella using better testing than was available in 2018 (Lyme Immunoblot, IgM/IgG, IgeneX Laboratories; Lyme PCR, T Labs; Bartonella FISH, IgeneX & T labs; ddPCR, Galaxy Laboratories; physical examination, looking for telltale Bartonella stretch marks or ‘striae’). The failures of our healthcare system denying care, while also denying tick-borne epidemics under our noses for decades, has led to an epidemic of long-term suffering, and may have played a role in what happened. If this were found to be the case, and he was treated for a potentially reversible mental illness, that could theoretically prevent more tragedies.
This horrifying scenario should prompt an open dialogue about the problems with our healthcare system. Approximately 1 of every 2 Americans suffers with a chronic health condition; 86% of our healthcare costs and 70% of the deaths in this country are due to chronic disease. Yet all we can do in our modern medical system is to “name the disease and throw a drug at it” without getting to the underlying reasons why people are getting sick. Pharmaceutical companies are the primary funders of medical school education training (shocking!) and teach doctors a model that no longer works well, because once patients are sick and chronically ill, it is essentially too late, increasing their suffering and associated healthcare costs. Patients suffer with long term symptoms, and even if the medicine is helpful (and I use a lot of pharmaceuticals that are lifesaving), we need to get to the underlying root causes of chronic illness before and after people get ill.
Our healthcare system is sick and needs an overhaul. As healthcare costs continue to rise, in large part due to pharmaceutical and insurance company profits, insurance companies too often deny absolutely essential care. (I recently read of one case where a person with melanoma in his eye needed a radioactive patch on his eyeball to treat it; his insurance covered the surgery to apply it but denied the surgery to remove it even though it had to be taken off. A radioactive patch! How depraved is that?) They hold onto money, accruing interest and increasing their billions of dollars of profits. They answer to their shareholders, not the people who pay their premiums and copays. Sometimes a pivotal moment in history opens up a dialogue that desperately needed to take place.
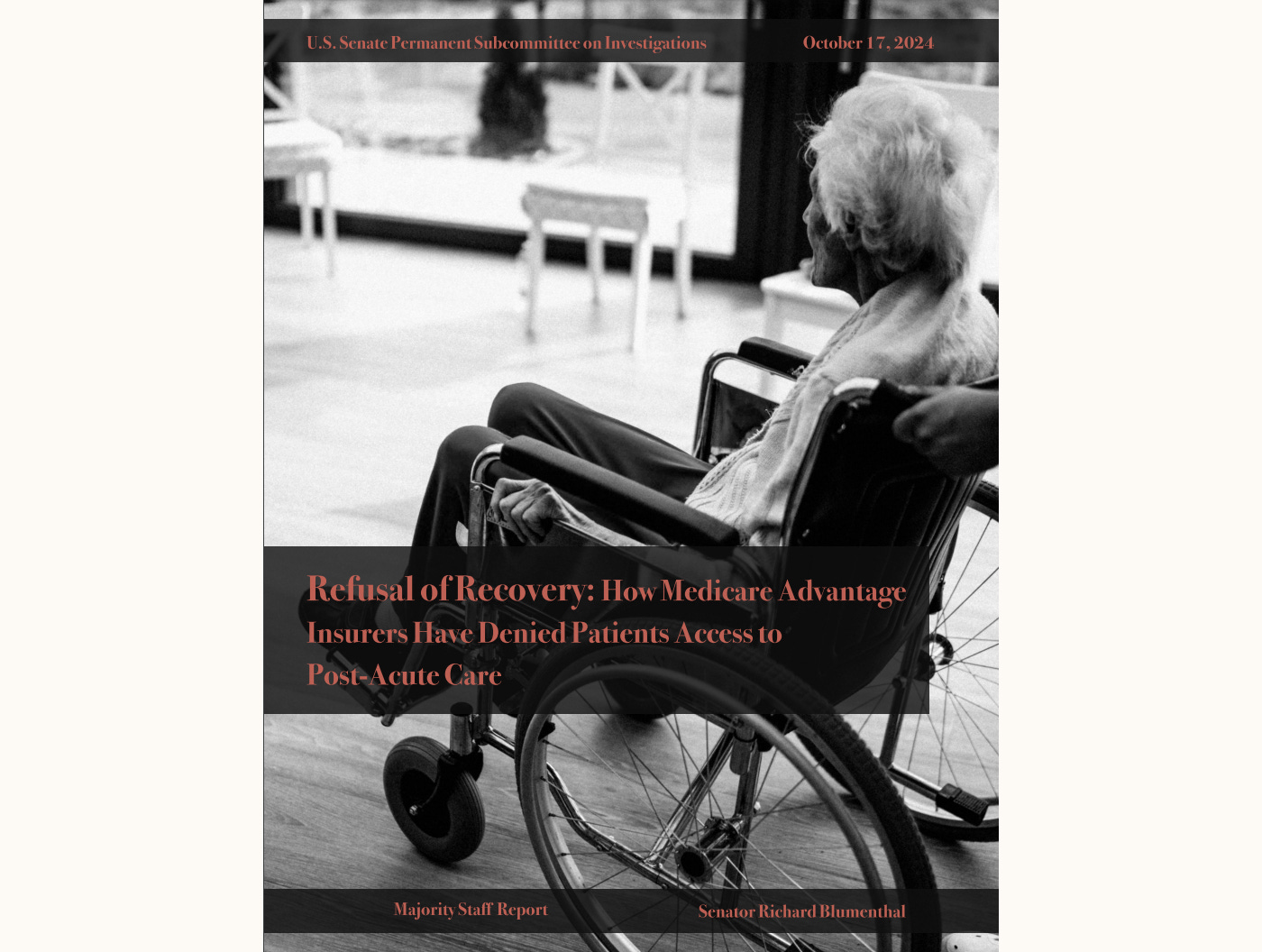
What are the facts surrounding insurance denials which lead to so much frustration among both doctors and patients? Federal data shows that health insurance companies denied more than 49 million claims in 2021, and these were appealed in a small percentage of cases. People are often too sick to fight with insurers and give up, and insurers know it. Investigative journalists at ProPublica found that the insurance company Cigna was using an automated system to assess, and often deny, claims in bulk.And a recent report by the U.S. Senate Permanent Subcommittee on Investigations released in October highlighted UnitedHealthcare's use of faulty AI to deny claims and found that the insurer's prior authorization denial rate for post-acute care jumped from 10.9% in 2020 to 22.7% in 2022. According to Health Leaders Media, UnitedHealthcare denies the most claims of any major health insurer, although data show and some industry reports show claim denials can range anywhere from 17% to 30% or more, depending on the insurance company. The way medicine was set up, it should be the patient’s healthcare provider who decides what is best for them, not a bean counter or bot from an insurance company. And even when medicines or therapies are medically necessary, they still are often denied.
Take my patient from two days ago who is overweight, with diabetes, hypertension, and hyperlipidemia. I prescribed semaglutide (a form of Ozempic, called Zepbound) to assist in weight loss, which he was unable to do with diet and exercise on his own. He is at risk for a heart attack, stroke, cancer, and Alzheimer’s disease because elevated blood sugars and insulin resistance underlie all of these processes. He is exactly the type of patient who deserves this treatment, yet it was immediately denied by the insurer, making my medical staff and nurses take precious hours of their time to go through the hoops to get it approved. I am paying my staff to do this, and a lot of my staff’s time is involved in more and more administrative work coming from insurers.
I hope this terrible tragedy leads to an open dialogue about how to change our dysfunctional medical system, getting to the root causes of illness and not just treating symptoms. This situation is driving up healthcare costs, which now accounts for 17.3% of our nation’s GDP.
The way to lower healthcare costs is not to deny necessary care. We lower healthcare costs through better prevention practices and getting to the root causes of why people are getting and staying sick. We need a full paradigm shift in the medical model of how we diagnose and treat chronic illness, and it makes a lot more sense to open up Prevention Centers of Excellence and Chronic Disease Centers of Excellence to focus on improving patient outcomes and lowering associated costs. We are finding that all 16 points on the MSIDS model that I use to diagnose and treat chronic Lyme have been found in many other illnesses including Long Covid and Alzheimer’s disease. When I do a medical search, looking up whether all 16 factors on the MSIDS model have been associated with a broad range of chronic illness, I find all of them are often published in the medical literature, showing an association. Association does not necessarily equate to causality, of course, but this approach needs to be investigated further. Using a multifactorial, personalized treatment model, and incorporating more prevention, would ultimately lower costs on the treatment side. There could even be incentives. The government could give back money on our taxes by meeting certain prevention standards and goals. Patients would be paid to stay well, going to prevention centers yearly (or more often depending on the illness/condition) and meeting standards of care. Doctors could be certified in comprehensive preventative care. Perhaps if people got money back on their taxes, giving them an incentive to stay well, we would have a downward shift in chronic diseases, as good health alone doesn’t seem to be enough….
I also hope we can use this tragic case to open another dialogue on how to shift the diagnosis and treatment of chronic illness in our country, including pain syndromes, and openly discuss the fact that infectious microbes can and do contribute to mental illness (which, again, may or may not have played a crucial role in this violent scenario). No one in the mainstream media is discussing this possibility.
But one thing is certain. People are mad as hell and aren’t wanting to take it anymore.
*References
Bransfield RC. Aggressiveness, violence, homicidality, homicide, and Lyme disease. Neuropsychiatr Dis Treat. 2018 Mar 9;14:693-713. doi: 10.2147/NDT.S155143. PMID: 29576731; PMCID: PMC5851570.
Abstract Background: No study has previously analyzed aggressiveness, homicide, and Lyme disease (LD).
Conclusion: LD and the immune, biochemical, neurotransmitter, and the neural circuit reactions to it can cause impairments associated with violence. Many LD patients have no aggressiveness tendencies or only mild degrees of low frustration tolerance and irritability and pose no danger; however, a lesser number experience explosive anger, a lesser number experience homicidal thoughts and impulses, and much lesser number commit homicides. Since such large numbers are affected by LD, this small percent can be highly significant. Much of the violence associated with LD can be avoided with better prevention, diagnosis, and treatment of LD.”
In 2024, Dr. Robert Bransfield and colleagues, including Dr. Monica Embers from Tulane, published an autopsy case of a homicidal individual in which they found active spirochetal infections in his pancreas and heart, with signs of brain inflammation:
Bransfield RC, Goud Gadila SK, Kursawe LJ, Dwork AJ, Rosoklija G, Horn EJ, Cook MJ, Embers ME. Late-stage borreliosis and substance abuse. Heliyon. 2024 May 11;10(10):e31159. doi: 10.1016/j.heliyon.2024.e31159. PMID: 38779029; PMCID: PMC11108998.
Abstract Background: Infectious diseases can contribute to substance abuse. Here, a fatal case of borreliosis and substance abuse is reported. This patient had a history of multiple tick bites and increasing multisystem symptoms, yet diagnosis and treatment were delayed. He experimented with multiple substances including phencyclidine (PCP), an N-methyl-d-aspartate (NMDA) receptor antagonist that opposes NMDA agonism caused by Borrelia infection. During PCP withdrawal, he committed one homicide, two assaults, and suicide.
Conclusions: Late-stage borreliosis is associated with multiple symptoms that may contribute to an increased risk of substance abuse and addictive disorders. More effective diagnosis and treatment of borreliosis, and attention to substance abuse potential may help reduce associated morbidity and mortality in patients with borreliosis, particularly in endemic areas.
Horowitz, R.I.; Fallon, J.; Freeman, P.R. Comparison of the Efficacy of Longer versus Shorter Pulsed High Dose Dapsone Combination Therapy in the Treatment of Chronic Lyme Disease/Post Treatment Lyme Disease Syndrome with Bartonellosis and Associated Coinfections. Microorganisms 2023, 11, 2301. https://doi.org/10.3390/microorganisms11092301
Delaney S, Robveille C, Maggi RG, Lashnits E, Kingston E, Liedig C, Murray L, Fallon BA, Breitschwerdt EB. Bartonella species bacteremia in association with adult psychosis. Front Psychiatry. 2024 Jun 7;15:1388442. doi: 10.3389/fpsyt.2024.1388442. PMID: 38911703; PMCID: PMC11190357.
Breitschwerdt EB, Bradley JM, Maggi RG, Lashnits E, Reicherter P. Bartonella Associated Cutaneous Lesions (BACL) in People with Neuropsychiatric Symptoms. Pathogens. 2020 Dec 4;9(12):1023. doi: 10.3390/pathogens9121023. PMID: 33291688; PMCID: PMC7761945.