Ticks are cesspools of germs. They contain multiple bacteria, viruses and parasites that can be injected into your body within minutes of a tick bite, causing long-term disability and even death if not treated promptly. The Powassan virus can get in within 15 minutes of a tick bite; Rickettsia rickettsii, Rocky Mountain Spotted Fever, can get in within 10 minutes of a tick bite. And the all-time winner is Borrelia hermsii, or Relapsing Fever, which can enter within 5 minutes of a tick bite.
And to complicate matters, one bite can potentially transmit multiple organisms, which is often the case with Lyme disease and Babesia. The two organisms have been found to have a high rate of co-transmission. That is part of the reason we see such high rates of Babesia in our sickest patients.
The most common ticks my patients are exposed to are Ixodes deer ticks (Ixodes scapularis on the East coast; Ixodes pacificus on the West coast, and the Lone Star tick (Ambylomma americanum).

The Lone Star tick has a characteristic white dot on its back and can come running from 50 feet away to bite you, even when you are not in high grass--a good reason to have tick protection with picaridin 20% on your skin and permethrin treated clothing! It can potentially transmit ‘TEARSv’ (tularemia, Ehrlichia, Alpha gal, Rickettsia and STARI [Southern Tick Associated Rash-like Illness] as well as viruses like the Heartland and Bourbon virus). Most of these are treated effectively with doxycycline if caught early, except for the viral infections, which can be deadly. Alpha gal can leave you with years of suffering due to allergies to red meat and animal products.
I sometimes see dog ticks and wood ticks that contain Rickettsia like Rickettsia rickettsii (Rocky Mountain Spotted Fever) and tularemia. Then there are new spreading ticks, that have come to NY, like the Gulf coast tick transmitting Rickettsia parkeri rickettsiosis (a milder form of Rocky Mountain Spotted Fever).
Ticks can contain bacteria, viruses, and/or parasites. In the Ixodes deer tick, we find:
Borrelia burgdorferi (Lyme disease)
Borrelia miyamotoi (Hard tick relapsing fever)
Anaplasma
Deer tick virus (Powassan virus)
Babesia (a parasite).
This Substack is about Babesia, but when I screen my patients, I find that other co-infections are the rule, not the exception. Babesia is suspected when patients present with a malarial-like illness with fevers, day and/or night sweats, chills (which can be shaking), flushing, and complaining of an “unexplained cough” and shortness of breath. When you take the Horowitz MSIDS questionnaire (HMQ), questions 1 and 22 are often positive when Babesia is present. See the prior Substack for more information.
Future Substacks will address some of the above infections, but I wanted to give you an idea of your risks when you are outside, highlighting the need for awareness and prevention. Since more than one infection can be transmitted by a tick bite, my advice is to send the ticks out to get them evaluated for infections if they have been on for more than several hours and/or are difficult to remove. Local health departments or specialized tick-testing companies like Ticknology are good choices.
Broad Testing Strategies Are Needed to Pick Up Babesia
The genus Babesia comprises more than 100 species of tick-transmitted protozoal pathogens (piroplasms). In the US, we primarily see Babesia microti & B. duncani (WA-1) as the 2 species making our patients ill. Rarely, other species can be present, including Babesia MO-1, KO-1, and potentially, a new kid on the block, Babesia odocoilei, an emerging species found in those who are chronically ill. Other parts of the world, like Europe, have different species, such as B. divergens (that frequently causes a hemolytic anemia), B. venatorum (EU-1), B bovis, B. microti, B. bigemina, B. major, B. Crassa, B. Occultans (8 in total).
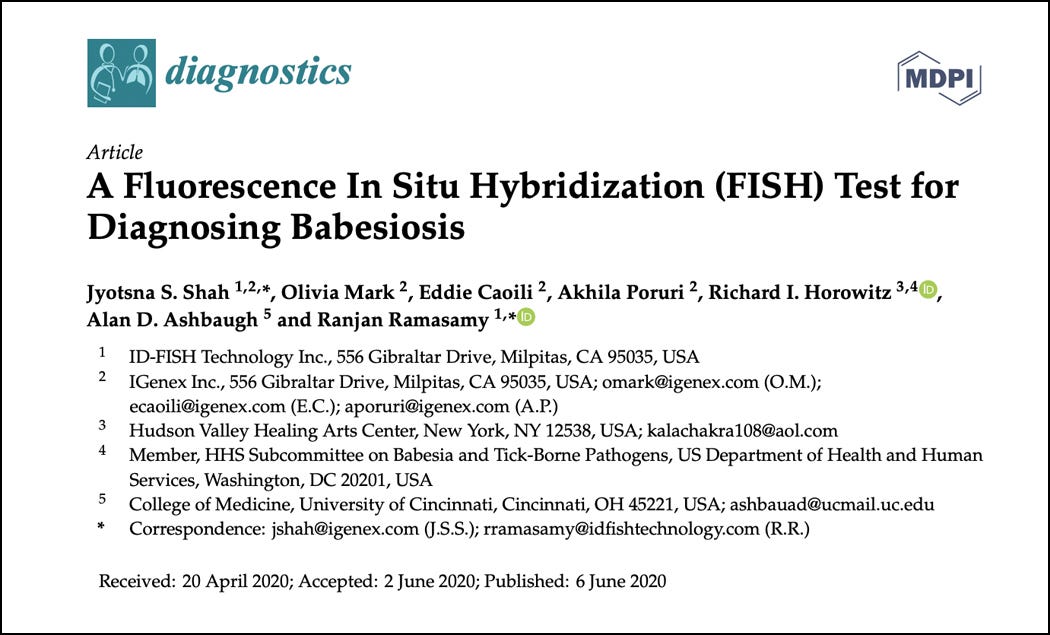
For that reason, a FISH (Fluorescent in Situ Hybridization) test that can pick up a broad range of Babesia species is a must, especially if patients have traveled to Europe and gotten ill. Also, a Babesia FISH test is essential in many of my US patients because some are immunosuppressed from Lyme and Bartonella, and they don’t make robust antibodies. Many times, antibody testing is negative for Babesia, and a FISH test is positive! Also, I have come to rely on FISH testing to prove ongoing infection after treatment. So, although we do use antibody testing for B. microti and B. duncani from local laboratories and get positives or do a Babesia Immunoblot IgM/IgG from IgeneX and find exposure, oftentimes just testing with antibodies is not enough. See the article below by Dr Shah, where I am co-author, on the usefulness of the Babesia FISH test:
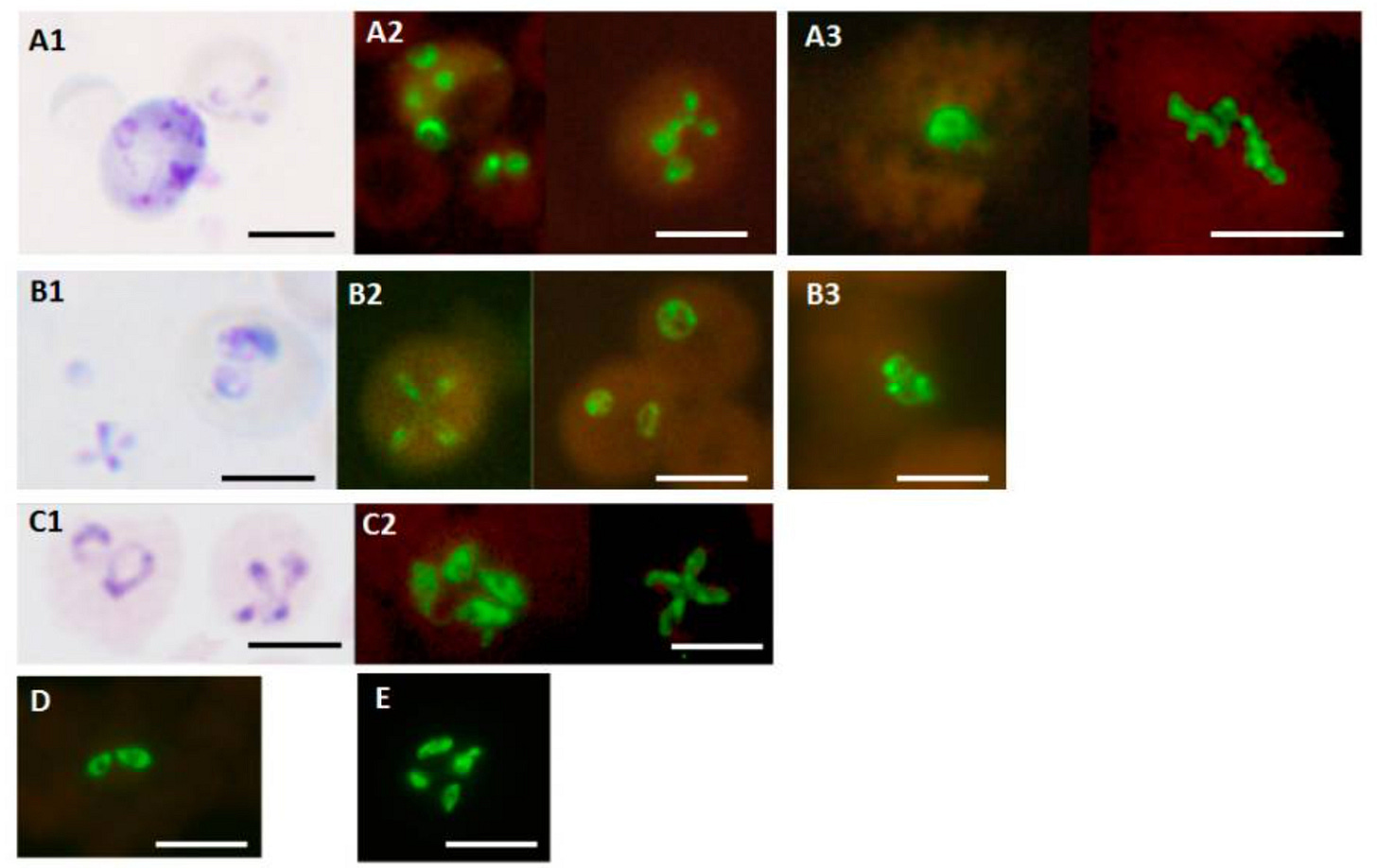
A T Labs Babesia FISH test will often find a positive B. odocoilei in our sickest patients with malarial-like symptoms. Although the presence and pathogenicity of this parasite is still being debated in the medical literature, you can see why just sending off antibody titers can be insufficient--and if they’re are on immunoglobulin therapy for immune deficiency, you can’t rely on antibody testing, as their treatment can give false positive tests.
That is why the Babesia FISH test from IgeneX and/or T labs is a standard test in my practice. It proves active infection, can check for multiple species, and avoids the pitfalls of negative antibody testing due to immune deficiency. You will find this information useful when your Medical Detective goes searching for proof of Babesiosis.
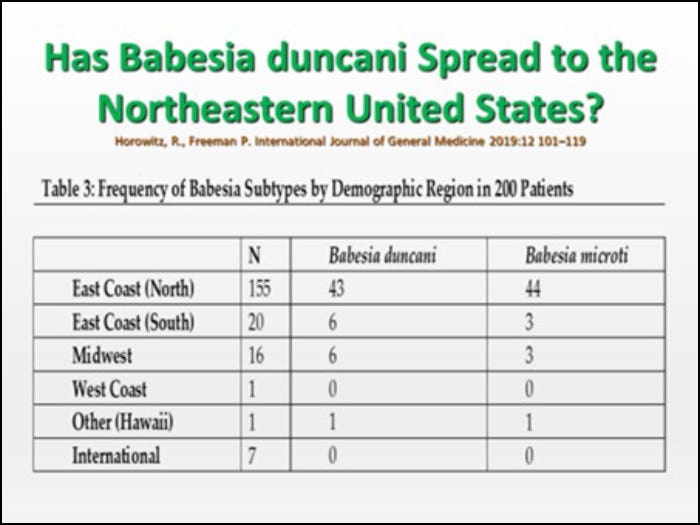
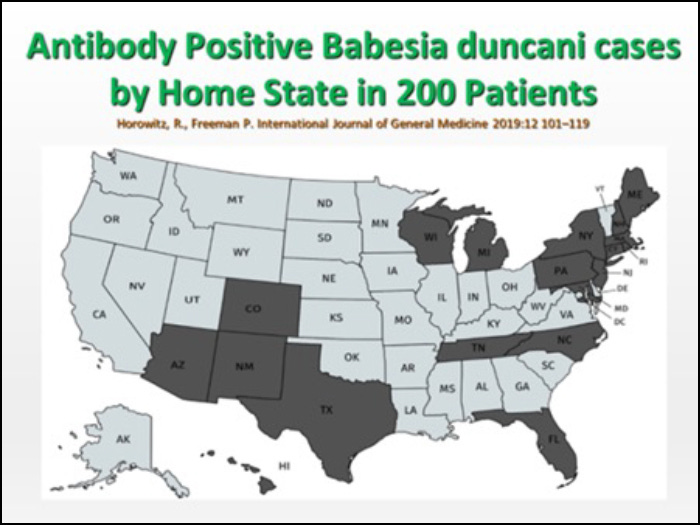
The other reason why you need to broadly screen for Babesia species, is that it is no longer just B. microti making people ill.
Although the CDC has only officially confirmed 14 cases of B. duncani, and it is not a reportable disease in all states, we are finding many more cases than the “official” counts. LabCorp and Quest diagnostics both have yielded positive B. duncani cases in my patients, but it is always possible that Babesia antibodies may cross-react and yield a false positive result. The Babesia Immunoblot from IgeneX laboratory is a good choice if you are concerned about the quality of the testing. This is a highly accurate Babesia test and is considered the gold standard for infectious disease testing because it's sensitive and specific and can detect multiple species in one test. The ImmunoBlot is more sensitive than other serological tests for Babesia, and it is specific, able to detect the full spectrum of disease, from early to late stages.
Another Reason to Screen? Chronic Persistent Babesiosis Is Seen in Seropositive Blood Donors Who May be Asymptomatic
Not all people with Babesia are ill. Some don’t know they have been exposed and have subclinical infections. A longitudinal study of Babesia microti infection in seropositive blood donors was performed, and 21% had evidence of persistent parasitemia. The study concluded that seropositive blood donors can have protracted low-level parasitemia that is variably and intermittently detected by parasitologic and molecular methods.
This is another reason we need to use a panel approach to test and suspect Babesia in those who live in highly endemic areas! Transfusion-associated Babesiosis is a well-known phenomenon, and in a prior study looking at 115,000 blood donations from the Midwest and New England, 4/1,000 transfusions were positive for Babesia. Some of those cases had atypical Babesia; in 2017, the fifth case of a B. divergens–like/MO-1 infection was found. Transplantation risk is also possible.
When Should You Consider a Giemsa Stain for Diagnosing Babesia?
If your healthcare provider does a Giemsa stain--the classic lab test for the parasite (a stain of the parasite under the microscope) --and it is negative, it’s probably because the level of Babesia parasites in the blood were not high enough to be seen (less than 5%). But there is a potential indication for this test: malaria.
Malaria is rarely found in the US, with cases reported only in Texas and Florida, yet it will become more common as temperatures warm from climate change—leading to an increase in mosquito populations. Anyone with malarial-like symptoms from those states should have a Giemsa stain to check for malaria. And if someone is in the hospital from a tick bite, and is severely ill with hemolytic anemia, the Giemsa stain will have a greater chance of picking up the parasite.
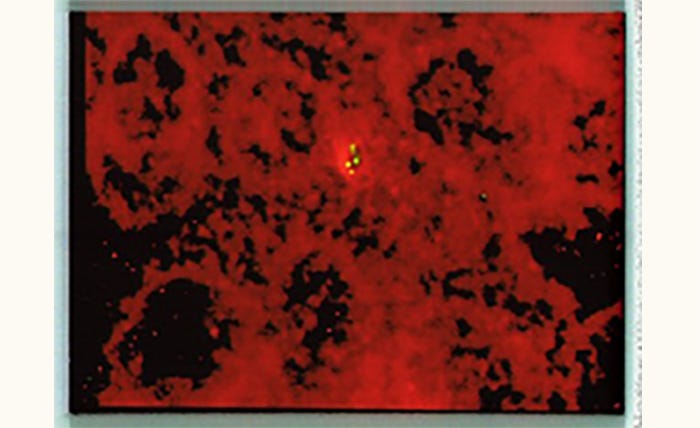
Malaria, like Babesia, is also spread via blood transfusions, organ transplants, maternal-fetal transmission, and unsafe needle-sharing practices, and the symptoms overlap Babesiosis with fevers, chills, headaches, fatigue, and nausea. Symptoms can occur 10-14 days post-exposure or show up one year later. A Giemsa stain for malaria will show “ring forms,” but in Babesia, a classical tetrad (Maltese cross form) will usually be seen. This image is of a positive Babesia FISH test from IgeneX.
Routes of Babesia Transmission
Infection by tick bite, blood transfusion, maternal-fetal transmission, and organ transplantation are the most common routes of transmission; there is also a remote possibility of transmission by fleas. Flea bites are a likely source of Bartonella in many patients (we are still debating ticks’ ability to transmit, although based on the number of sick individuals with the 3 Bs, Borrelia, Babesia, and Bartonella, it is likely). A 2020 study showed that in Pennsylvania, fleas contain Babesia as well as Rickettsia.
The Medical Detective would suspect Babesia when a Lyme patient has particularly severe symptoms because, like Bartonella, Babesia increases the severity of all symptoms. These can include fatigue, joint/muscle pain, headaches, neuropathy, emotional and cognitive difficulties… but the best clues here are the malaria-like symptoms: fevers, chills, flushing, and day and/or night sweats (mild, moderate, severe). Other symptoms might be hemolytic anemia, thrombocytopenia (low platelet counts), and elevated kidney function (increased BUN/Creatinine) but these are rarely seen in my patients unless they are immunocompromised and missing a spleen or have B. divergens, the European strain most associated with the red blood cells breaking apart (hemolysis). Severe hemolytic anemia can be found in patients with normally functioning immune systems and intact spleens, but usually is seen only in very young or elderly patients with other chronic medical problems. Looking for EBV and/or liver disease with cirrhosis if you have an enlarged spleen is something to consider since I don’t see enlarged spleens in the majority of my chronically ill Babesia patients.
Atypical Symptoms of Babesia: Cardiac and Neurological Complications
An unexplained cough and air hunger (the feeling of not getting enough air into the lungs) are frequently seen in my patients suffering from Babesia—but a rare complication is also occasionally seen in hospitalized patients with severe illness, where they have a white-out of the lungs on a chest-X-ray and difficulty breathing with poor oxygenation. This is called ARDS (acute respiratory distress syndrome). This unusual manifestation can be seen in other illnesses, like malaria, severe Covid (early in the pandemic we saw a lot more of this), and even Relapsing Fever Borrelia, but there can be other reasons for these respiratory symptoms in our patients. A comprehensive workup is needed to rule out allergic rhinitis with a postnasal drip, asthma, and reflux, which are the other common causes (in 99% of cases). There are of course other reasons for an unexplained cough and shortness of breath, ranging from lung cancer, pulmonary infections and fibrosis, interstitial lung disease, etc., but in day-to-day medical practice, a chest-X-ray can help rule out these other diagnostic possibilities if warranted.
Some unusual symptoms of Babesia have been reported in the medical literature in the past few years, and the Medical Detective needs to know all the potential complications.
Cardiac complications of Babesiosis can include new onset of atrial fibrillation (many patients are now picking it up with Apple watches), atrial tachycardia, ventricular tachycardia, congestive heart failure, ARDS, and a prolonged QT interval on the electrocardiogram. This is not regularly seen in my patients, but greater than one-third of hospitalized patients with B. microti can develop these severe cardiac complications. In severe cases, ARDS, disseminated intravascular coagulation, severe hemolytic anemia, coma, shock, renal failure, splenic rupture, and death are all possible.
Neurological complications of Babesiosis can lead to confusion, cognitive impairment, slurred speech, and balance problems (ataxia). One of the reasons is that both malaria and Babesia can cause inflammation in the brain. Steroids should be avoided in these patients, as they can cause reactivation of latent Babesia infections, and some people have died after receiving high dose corticosteroid therapy. So before giving immunosuppressive therapies, like steroids or Rituximab, which decreases the B cells that make antibodies, check if patients have Babesia or other underlying infections. Immunosuppressive therapies used in certain autoimmune diseases can reactivate parasites like Babesia, bacterial infections like tuberculous, or cause lymphoma.
Babesiosis in Pregnancy
I’ve encountered this situation several times during the 40+ years of my clinical career. Mothers with prepartum Lyme + subclinical Babesia can potentially transmit the infection to their fetuses. If so, the newborn may require a transfusion if they weren’t treated prior to birth because they can develop hemolytic anemia and jaundice. Not a great way to start childhood! Fortunately, I’ve never seen this complication happen because I’ve picked up Babesia before delivery and treated when appropriate.
All pregnant women should be checked for Lyme and associated co-infections. Lyme, Babesia, Bartonella, Relapsing Fever Borrelia, and rickettsia can all be transmitted from the mother to her baby. We suggest using the HMQ before pregnancy. My patients are automatically screened for Babesia when they fill out the validated Horowitz Lyme symptom questionnaire, which can be downloaded from my website: https://cangetbetter.com/wp-content/uploads/2021/02/MSIDS-QUESTIONNAIRE-FINALR.pdf
Treatment in pregnancy usually involves 2 primary treatment options. The first, published in the New England Journal of Medicine in 2003, is oral Clindamycin 600mg 3 times a day (TID) and Quinine 650 mg TID for 7 days. That regimen has been shown to be effective and safe in the third trimester, but can’t be used in the first 2 trimesters (high dose quinine can cause an abortion in the first trimester). I don’t like using quinine because of the potential side effects of nausea, vomiting, severe ringing in the ears, and, occasionally, rashes, apart from the drug being able to prolong the QT interval on the electrocardiogram. I used to joke with patients that if they don’t behave, they will get this treatment!
The regimen that I prefer, which we published in the medical literature a few years back, is using Clindamycin 600 mg TID + Mepron (atovaquone, 1500 mg twice a day) & Zithromax 250 mg twice a day for 10-14 days. This can safely be used in the third trimester, and when we gave it to a mother who was Babesia FISH positive in 2 out of 4 consecutive pregnancies, this regimen resulted in healthy babies.
This patient was from Europe and not only had an EM rash, the pathognomonic rash of Lyme disease, but she also had a violaceous skin rash on her hands--ACA, or Acrodermatitis Chronica Atrophicans. This rash is caused by a European species of Borrelia, B. afzelii, and is a chronic persistent Borrelia species. (Skin biopsies years later have proven active infections in some of these patients.) She decided to do intramuscular penicillin injections (Bicillin LA) twice a week during all 4 pregnancies to protect her children from maternal-fetal transmission, and they were all well and free from infection at birth. We regularly do cord blood analysis at birth to look for Lyme, Babesia and occasionally Bartonella, and fortunately, even though the cord blood will occasionally have a positive PCR for Lyme, or be FISH positive for Babesiaor Bartonella, the children have remained healthy when followed by their pediatricians, as long as the mother received treatment during pregnancy.
One of the differential diagnoses that the Medical Detective must consider in pregnancy in a patient with hemolytic anemia is a syndrome called HELLP Syndrome. This stands for Hemolysis, Elevated Liver functions and Low Platelets. The symptoms are like those seen in Babesiosis but is an autoimmune phenomenon and treated differently.
Problems with Babesia Treatment
Babesia can persist after short-term and long-term treatment in co-infected Lyme patients. Rotations of antimalarial medication and herbs are often necessary. Next week, in the third and final series of the Medical Detective Substack, I’ll discuss details of how I treat resistant Babesiosis in my practice. Stay tuned!