The barbecue’s fired up and you can’t wait to throw on some burgers (free range, of course) and knock back a cold beer. Your friends arrive for a joyful afternoon, but 4 hours later, one of them starts to choke and has difficulty breathing, develops a rash, and suddenly doubles over with abdominal pain, nausea, and vomiting.
No, it wasn’t your cooking or tainted beef. Welcome to Alpha Gal Syndrome (AGS), an allergic reaction. It’s already affecting approximately 500,000 Americans. It’s spreading. And it’s likely to get worse.
What causes AGS? Ticks. Just as ticks are emerging in warmer weather, the CDC reported last week that lone star ticks (Ambylomma americanum) are not the only ticks that transmit AGS in the US. Two other species, the blacklegged deer tick (see below) and Western blacklegged wood tick, are also implicated. which can also trigger the allergy.

That other ticks can transmit AGS increases the risk for everyone to develop this potentially life-threatening reaction to a tick bite. Most cases of AGS have been in the eastern, southeastern, and south-central parts of the US, but this new case report expands the areas where you are now at risk.
Diagnosing AGS
AGS is an allergy to mammalian meat and products derived from mammals, caused by immunoglobulin E (IgE) antibodies against a sugar molecule (carbohydrate) in our bodies called galactose-alpha-1,3 galactose (alpha-gal). A diagnosis can be made after the following:
1. Clinical History: Patients often report a delayed allergic reaction (2-6 hours after ingestion of mammalian meat (beef, pork, lamb, organ meats) and sometimes gelatin and dairy products. Symptoms can include:
Skin: flushing, itching, and hives, as well as swelling of the face, lips, and tongue.
Gastrointestinal: nausea, vomiting, diarrhea, and abdominal pain.
Respiratory: asthmatic-type symptoms with wheezing, shortness of breath, and a cough. In severe cases, anaphylaxis can result, characterized by low blood pressure and fatigue, dizziness, a rapid heartbeat, with swelling of the tongue and/or throat.
Not everyone may get these reactions. It’s important to note that symptoms can vary in severity; for some, the symptoms are mild, such as hives, while others may develop severe anaphylactic reactions.
2. Blood Testing: Measuring specific AGS IgE antibodies in the blood is crucial to establish the diagnosis. This is because other food allergens like peanuts can cause similar reactions, and you need to know what the trigger or triggers were. Positive testing with AGS IgE Antibodies to alpha-gal supports the diagnosis, but must be interpreted in the context of clinical symptoms. Why? Some people may have elevated AGS IgE without symptoms. What do we do with those who test positive? Two things. An avoidance diet, and broaden the differential diagnosis to include other causes of hives and allergic reactions.
3. Dietary Elimination and Challenge: anyone suspecting they may have AGS need to follow an alpha-gal avoidance diet, eliminating all mammalian meat and related products for at least a month. Symptom resolution on this diet further supports the diagnosis. Reintroduction of mammalian products under medical supervision can confirm the diagnosis if symptoms occur.
Differential Diagnosis for AGS: Food allergies, MCAS, Environmental Allergens
Anaphylactic/allergic reactions can come from 2 other major sources which need to evaluated. Food allergies, such as peanuts, as you just read, can mimic AGS, due to their potential to cause anaphylaxis and other allergic symptoms—but they typically cause immediate reactions (within minutes to 2 hours) after ingestion. AGS reactions, on the other hand, are delayed, occurring 2-6 hours post-ingestion of mammalian meat. Getting an IgE food allergy panel to assess common food allergens, like peanuts, dairy, wheat, corn, shellfish, etc. can help establish the role of other food triggers, along with getting skin prick testing (RAST) through an allergist.
Mast cell activation syndrome (MCAS) can also present with symptoms similar to AGS, including urticaria, gastrointestinal symptoms, and anaphylaxis. MCAS can affect every organ system in the body, but does not have a specific trigger like mammalian meat ingestion and is usually more chronic and recurrent in nature. An MCAS diagnosis involves demonstrating elevated levels of mast cell mediators like tryptase, chromogranin A, histamine, and PGD2. People who suffer from leaky gut and intestinal barrier dysfunction with increased intestinal permeability often have mast cell reactions with delayed hypersensitivity reactions. Doing a 95 IgG4 delayed food sensitivity panel with zonulin levels can help to establish leaky gut as an underlying source of MCAS. (Lyme disease, mold toxicity and even Long Covid can trigger MCAS too and need to be included in the differential diagnosis).
Other Unusual Sources of Allergic Reactions and Asthma Attacks
And then there are cockroaches. According to Dr Cheryl Burdette, who runs Precision Point Diagnostic laboratory: “Studies have shown that exposure to cockroach allergens is a major risk factor for asthma morbidity in inner-city children. The prevalence of cockroach allergies varies, but it is estimated that a significant portion of asthmatic children in urban areas are sensitized to these allergens. Arguably, cockroach allergens are the most prevalent indoor allergens and may be the ones that have the greatest impact, possibly excepting molds… Cockroach allergy is an important risk factor for hospital admissions, emergency department visits, and asthma morbidity, exerting a greater impact on the latter than dust mites or pets. The prevalence of cockroach allergy ranges in the United States from 17 to 41%, while in Europe 25% of asthmatic children are sensitized to cockroaches. Allergens from cockroaches are detected in 85% of homes in inner cities in the United States, where 60–80% of asthmatic children show a positive prick to cockroach extract.”
Since cockroach allergens can remain airborne for months inside a home, this is an allergic source that easily be missed when there are no visible roaches. Since cockroach antigens are missing from allergy skin tests, we need other ways of determining exposure and risk. The Precision Point Airborne Allergy Test measures the body’s immunoglobulin E (IgE) response to 85 common airborne allergens, including cockroach, pet dander, mold, dust mites, grasses, crops, trees, and weeds.
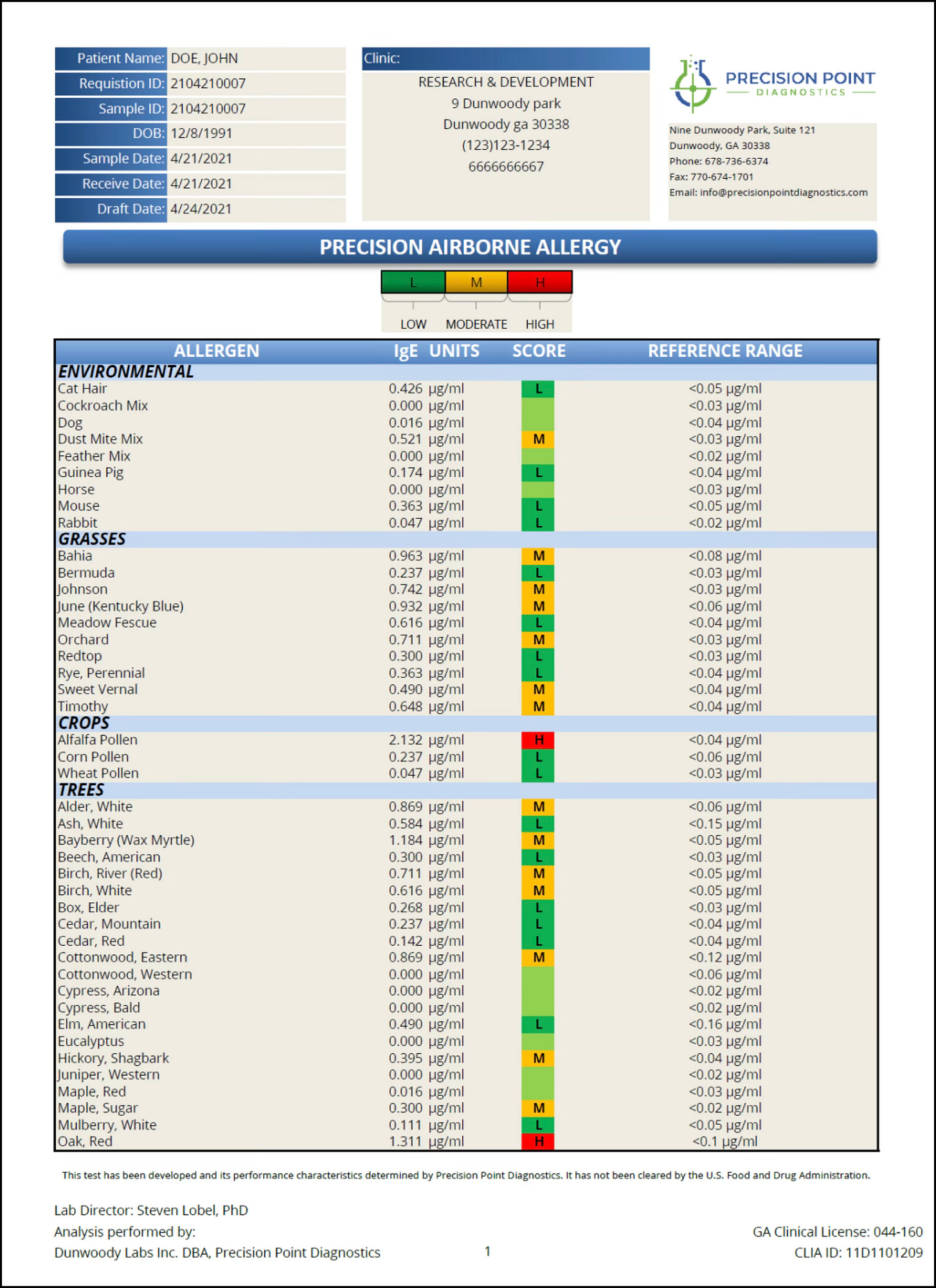
This serum test can be used with skin prick tests and should be part of a comprehensive workup when severe allergies/asthma/anaphylactic reactions take place.
Treatment Options for AGS, MCAS, and Allergies
The best treatment for AGS involves a combination of dietary management and preventative measures. This means strict avoidance of mammalian meat and products derived from mammals, including beef, pork, lamb, venison; products such as lard and gelatin; and certain dairy products, particularly those high in fat content like ice cream and cream cheese. Fish, seafood, poultry, turkey and other non-mammalian products are generally safe for consumption. You need to read food labels very carefully, and avoid cross-contamination in restaurants and processed foods.
In cases of accidental exposure, acute management involves the use of anti-histamines like Benadryl (diphenhydramine), an H1 blocker, with Pepcid (famotidine) an H2 blocker, as well as having access to a Medrol dose pack (short course of steroids) and an Epi-pen, if there is concern for anaphylaxis. Dupixent (dupilumab), a monoclonal antibody, approved for conditions like atopic dermatitis, asthma, and chronic rhinosinusitis with nasal polyps, is being considered in severe cases, since it addresses type 2 inflammation, a key factor in allergic reactions.
For those with overlapping food sensitivity/allergies and MCAS, regular use of a non-sedating anti-histamine (Allegra, fexofenadine; Claritin, loratadine; Zyrtec, cetirizine) and an H2 blocker like famotidine can be helpful, along with Singulair (montelukast), mast cell stabilizers like cromolyn sodium (Gastrocrom, NasalCrom), and compounded antihistamines like ketotifen, which also functions as a mast cell stabilizer. Mast cells are immune cells that play a crucial role in allergic reactions and inflammatory processes, and are found in tissues/sites exposed to the external environment like the skin, lungs, and GI tract. By using a combination of medications that block histamine and mast cells, we can improve symptoms.
Helpful nutraceuticals include quercetin, PEA, luteolin, resveratrol, curcumin, and butyrate. Quercetin helps inhibit mast cell degranulation and cytokine release, making it more effective than cromolyn sodium! Resveratrol, a polyphenol in grapes, inhibits mast cell activation by suppressing key inflammatory pathways, as do curcumin and luteolin. Butyrate, a short chain fatty acid, helps manage mast cell activation by decreasing histamine levels and modulating mast cell function. It also supports gut barrier integrity, is an energy source for cells lining the colon, has anti-inflammatory effects and modulation of immune function. All of the above can be used in severe cases. Remember, you can have more than one reason why you suffer from allergies and severe allergic reactions, and all of the above factors should be looked into.
Tick Avoidance Is Essential To Prevent AGS and Exacerbate Sensitization
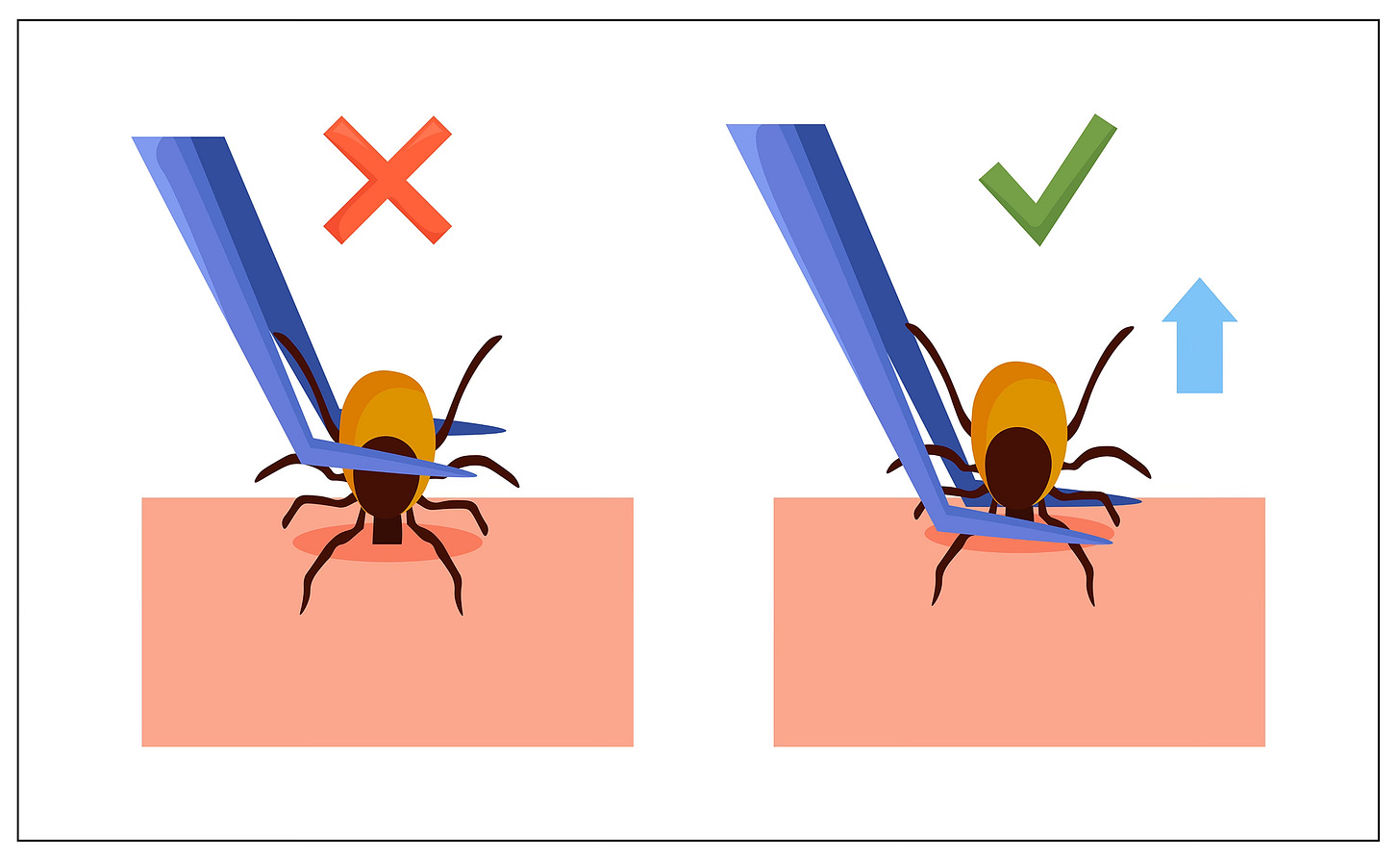
The only way to avoid AGS is to avoid getting bit by ticks. Tick repellants like picaridin 20% on the skin is my favorite, but others include IR3535 (safe in pregnancy), lemon-eucalyptus oil, and DEET 20% for deep woods (avoid it in young children). Permethrin-treated clothing will also kill ticks.Do regular tick checks when outside and immediately remove ticks with a fine pointed tweezer, pulling directly up from the skin if a tick starts to embed. Do not squeeze the tick, burn it, or put chemicals on it, which may cause it to regurgitate bacteria, parasites, or viruses into the skin. Once inside, taking a shower to check for ticks, and putting your clothes in the dryer at high heat for 10 minutes, will kill ticks.
Another Tick to Watch Out For
In other parts of the world, the Asian long horned bush tick, Haemophilus longicornis, has been known to transmit AGS.
We will likely have a big problem with this tick in the US in years to come, which is a hermaphrodite (it can reproduce on its own without a mate), allowing it to spread rapidly. It is now in 21 states and Washington, DC. Although there are no known associations between this tick and AGS in the U.S. to date, that doesn’t mean it won’t transmit it in the future. Pathogens detected in this tick in the US include a parasite that causes bovine theileriosis, a disease affecting cattle; Rickettsia rickettsii, the bacteria responsible for Rocky Mountain Spotted Fever (seen in laboratory settings), Borrelia burgdorferi (Lyme disease) and Anaplasma phagocytophilum, the agent causing HGA, Human Granulocytic Anaplasmosis. Viruses found in this tick include the Heartland virus and SFTS, Severe fever with thrombocytopenia syndrome virus.
So if you do get bit by an Asian Bush tick, it is unlikely you will get sick from AGS or the above infections in the US (the risk is higher in Asia), but just as Ixodes ticks and the Western blacklegged tick are not typical vectors of AGS, the science is evolving and so are these ticks.
There are more dangers to Ixodes/deer tick bites than we previously suspected. Stay safe!
Dr Cheryl Burdette will be interviewed by me for the Healing Lyme Summit 2.0, which airs April 15th-22. It is free to attend. Come hear Cheryl discuss how to use functional medicine testing in the difficult to treat Lyme patient! The link is below to sign up: